It is no secret that demand far exceeds supply in the world of fertility treatment, a gap franchises like Mate Fertility seek to close. But REI’s, like Dr. John Storment, argue that the training process employed by organizations like Mate merely imply board certification, and oversimplify years’ worth of education and training. Traci Keen believes that her company is serving the needs of patients with integrity and diligence, providing access to care that would be otherwise unavailable due to the lack of board-certified REIs in existence.
Who is right? Is access to care, even if it is not in line with ASRM guidelines, better than no care at all? Is this the evolution of fertility patient treatment?
Listen to the latest episode of Inside Reproductive Health to learn:
How impactful the care-access gap is to the evolution of fertility treatment.
Griffin press on the difference between private equity and venture capital’s place in the industry.
Dr. Storment discuss how fellowship training in REI is absolutely necessary and OB/GYN physicians cannot be equally trained in mini-programs provided by organizations like Mate.
Traci Keen argue the criticism of Mate Fertility’s training program, how they provide an evolved model of care, and how they plan to increase accessibility of treatment.
Traci's Information:
LinkedIn: https://www.linkedin.com/in/traci-keen/
Website: www.matefertility.com
John's Information:
LinkedIn: https://www.linkedin.com/in/john-storment-b4892b1b8/
Transcript
[00:01:40] Griffin Jones:
About darn time Inside Reproductive Health audience about darn time, all the emails that I've gotten from you over the years, the texts that I've gotten from you over the years, when someone on the show says something you don't like. And then I say, oh, Dr. So-and-so or Mr. Ms. So-and-so would you like to come on and share that point of view and almost always is declined.
Finally, add two people willing to come on. And have it out in a discussion. Traci Keen is the CEO of Mate Fertility. We interviewed one of their co-founders. Gabe Bogner a few months back as you may remember a Dr. John Storment he's been on the show before too. He owns a practice in Louisiana whose lab was owned by Ovation Fertility, and we get into the discussion of access to care versus.
The necessary credentialing for fertility specialists. I've tried to separate those two issues as best as I can because those two issues intermingle with each other, but they have to be discussed separately. I think my electrician analogy works in that case, but you let me know. Where do you side on this?
What do you think from the arguments that were made? Kudos to both my guests for coming on. And hopefully we can have a lot more discussions like this in the future. But what do you think, where do you fall on each side of the debate?
Ms. Keen Traci welcome to Inside Reproductive Health. Dr. Storment John. Welcome back to Inside Reproductive Health.
[00:03:11] John Storment: Hello Mr. Jones. Griffin.
[00:03:14] Griffin Jones: So Johnny emailed me when I had released an episode with Mate Fertility. And you had some concerns about the model and what was it that made you want and for, well, first off, before I even go there kudos to both of you for coming on the show, because I have a lot of guests on the show and sometimes people email me and they're like, ah, I don't like that idea.
Or that idea is in sounded good to me. And I said, well, come on the show then. And almost always. No, nevermind. And so kudos to Dr. Storment for actually coming on the show, kudos to Traci for coming on to, to answer any questions. But John, what is it that you wanted to respond to?
[00:03:52] John Storment: Well, I think that the key point is when I see the industry, the private equity and venture capital enter in our industry we have to look sort of with the keen eye to see, is this going to improve the delivery of care or is it going to hurt or potentially worse than care?
My concern for this is that your, I mean, gaves entire podcast, almost. He talked about how we overcomplicate the fertility space and that it's a whole lot simpler than we make it look. And I spoke with several of my colleagues and my concern is two-fold number one. They say that they're mission is to decrease costs and increase access. And yet the first clinic they put, they put it in a, you know, an area that has a plethora of REI is in the university and also in private practice in Oklahoma City. And then their cost is exactly the same as our costs. And then they say, well, we want to, we want to enter the space and put a bunch of general OB GYN after a short training course.
And it essentially it seems like that our entire specialty is about editorials and transfers and not identifying the reproductive. Medical problems and our specialty. And I think that as a group we have to sort of stand up for not, not for defending our space. That's not it, that's not it at all.
It's we have to say that what we do is not uncomplicated. What we do is very complicated. And so when this podcast came on, there were a whole host of comments made by the group of that are just not correct. And so that's kind of what made me stand up and say I've since talked to some of my colleagues and there's, there are a lot of people around who agreed with that.
[00:05:46] Griffin Jones: Well, let's start with the first one. Cause there's a couple points in there we can get to the deep, to the cost, but I do. And you know, maybe it's a poor choice of words and I said that to gave us like, well, it is kind of that complicated, but let's go with that point, Traci is that there's a reason or at least assumably, there's a reason that this is a subspecialty and that a board accredited and that people have to do three years of training. So what about this concept of, of this re this it's not over-complicating it really is that complicated. And maybe not just any physician can do it.
[00:06:23] Traci Keen: Sure. Yeah. I think one of the main things to look at is that the way that our model is actually built, we are very much honoring what REI is bringing to the table.
We have a number of REI that we work with in our tele fertility model. And. We are partnering with OB GYNs because one of the fundamental issues, if you look at few different sides of this problem, we'll call it is access and it's access for all folks, not just you know the folks who typically receive care but in general. And so what we're actually doing is providing the initial lift training to upskill, OB GYNs, to perform retrievals and transfers under the supervision and ongoing quality care and control of a qualified REI, board certified REI.
[00:07:17] John Storment: Oh, there's board certified RIA is going to be in that clinic supervising them.
[00:07:22] Traci Keen: Well, I guess to that specific question I would love to know sort of in your model, I know that you're not the only staff member and I do believe you have an OB GYN on staff. Are you in the room every time they're performing any type of fertility related service for your patients?
[00:07:38] John Storment: Who is the OB GYN that I have in my model?
[00:07:41] Traci Keen: I believe you had an OB GYN listed on your website.
[00:07:44] John Storment: If I had two OB GYN, or they were just general GYN as they didn't do any fertility, they did just GYN. One of them has passed away. One of them is retired. So, no, I don't have any,
[00:07:54] Traci Keen: My larger point would be that there are only two countries in the world that require a fellowship.
Now we're not saying that we don't want to honor that and utilize that.
[00:08:03] Griffin Jones: Well, there's two countries in the United States in Canada.
[00:08:05] Traci Keen: That's correct. So we're not saying that the information in the fellowship is not valuable. We're actually saying quite the opposite, but what we are saying is let's enable everyone to practice at the top of their license and utilize REI is in a more strategic and efficient way to oversee the part of the care.
As you said, you know, it is very complicated. I think it would be you know, but what we're trying to do is enable REI to provide initial and ongoing upskilling to OB GYNs. However, those OB GYNs are not just practicing Willy nilly on their own. After the initial upskilling there's ongoing quality control and analysis.
On behalf of our team, we have an advisory board, there are monthly meetings to do QA there's daily touchpoints between an REI and during the protocol management process. We have IVF coordinators. We have you know, multiple REI is involved not only in the standard of care review, but also in retroactive review of all things that have happened.
So what we're trying to solve for is really that, you know, 42 REI's are graduating fellowship. I believe on an annual basis, somewhere around that. And when we look at the disparities in the market for the need versus the demand, the demand for care versus the supply, it's simply not there. So rather than focus on, you know, who's right or who's wrong, what we're trying to do is come up with a solution that will meet the need of people who actually need care in.
[00:09:44] Griffin Jones: We do have to focus on it. We do have to focus on that because access to care is an issue. And I do, and I'm going to press Dr. Storment on that, in this conversation, but it's also separated from who's qualified to do it. There's a shortage of electricians.
There's a shortage of plumbers out there. If. We can only assumably lower the licensure, whatever the requirement is to be a master electrician, a journey electrician so much before there's fires and everything. It doesn't, it doesn't change the problem that we need more electricians. And that there's a huge shortage there.
But what about, so, John, what about Traci's point of that level of supervision? What makes that inadequate in your eyes?
[00:10:26] John Storment: Well, so you over simple, they're oversimplifying it way, way, way too much. And here's why. Patients don't come to my door and say, Hey, I'm a simple infertility patient. We just need IVF.
And, you know, we're going to be easy. We're going to get 15 eggs and we have no other complicating factors.
[00:10:45] Traci Keen: I don't think that anyone on the Mate team is actually saying, this is going to be easy. We actually take what we're doing quite seriously from patient intake, all the way through it.
[00:10:55] John Storment: Absolutely, Gabe says that. Gabe said we don't want the complex.
We want the simple, and so let me finish my point. When a patient comes to me she doesn't come to me and say, I'm simple or uncomplex, it takes a thorough history. My three years of fellowship in 25 years of experience, not identifying teaching me. How did those, it didn't take me that long to learn how to do a retrieval and transfer.
I absolutely do not think that a retrieval and transfer takes three years to learn. I am saying that. The complexities and reproductive medicine don't show up easily and it takes years of experience and it takes our fellowship to identify this. Your OB GYN who has a week long training course in Mexico.
And then coming back up to here does not have the training to identify those complexities. I had a patient yesterday this morning. She had, she has had a tubal ligation, and she has four year point number that she just failed to you. A number of transfers amongst the simplest case there. And she has a lot more complex things going on that are not going to be addressed by a general OB GYN, no matter how many touch points you have, simply you're, it's just not able to be taught.
in a week-long course.
[00:12:17] Traci Keen: It's not a week-long course. It's actually quite a bit more significant than that. And it's not only, I'm sorry. So let me finish what I was saying. It's actually not a week-long course. It's an extensive remote learning and also onsite training. We do not at any point announce now we're not sending people to Mexico.
That was someone that we were working with prior. We've actually restructured quite a bit internally including myself and one of the things that is really important to us. You know, when I look at the fertility industry, I went to college with the first IVF baby ever born in the United States of America.
So when you're looking at me, you're looking at the exact age of this practice in the United States and what we're trying to do in reality, versus I think the picture that you're trying to paint by what you're saying, without understanding the full picture of our education program and our ongoing support and education.
What we're trying to do is acknowledge that this is an ever evolving industry. This is an industry where there needs to be a lot of quality control. So we're trying not only to increase access by upskilling people to participate in tandem with REI. We're not saying go out there on your own OB GYN and practice and just do it on your own.
That's not what we're saying at all in fact.
[00:13:40] Griffin Jones: So go into a little bit more I'm cutting you off Traci, because I want to keep us on this point. Please go into a little bit more detail of the training that you all do because somebody else, a different physician in a completely different part of the country for all I know, doesn't even know John texted me the same thing. What are you doing? Having on somebody that trains their people in Mexico. So please clarify what it is that you all do for your training programs.
[00:14:03] Traci Keen: Yeah, sure. So we actually, we have an LMS and we have 250 hours of required learning that actually have testing as they go along.
That's in the initial wave and we are constantly creating new materials for that LMS. And then we have a facility that we've partnered with for observations to occur for education. And then when it's time we also have a licensed professional go on. To train in person with them. And we also have our Oklahoma facility where people can also visit as well.
So we're not doing anything outside of the country at this juncture that actually predates my existence with the company. So you know, that's one of the things that is important, you know, we, we take quality of care incredibly seriously. And so does everyone who's involved with this company at this juncture.
You know, I think if you look through our roster currently, we have pretty extensive experience of some very well-respected people in the field who also see the issues in the field and the, you know, typically. And one of the things that Dr. Storment mentioned is, you know, when private equity or venture capital goes into a space, typically we see three things happen.
We see increased access, decreased price, and higher quality of care or standardization of care. Well, we're not typically seeing those things particularly in the fertility market, you know, costs aren't going down, access isn't increasing. In fact, it could arguably be decreasing slightly because we have a wave of REI who are about to retire, which is going to further constrain the already constrained supply.
You know, when you're looking at a population estimates are 30% if you're including LGBTQ genetic disorders in need of fertility care and only 2% receiving, you know, to me, that's a big problem. And instead of focusing on divisive things, you know, why are you doing what you're doing? You know, we are mindful, incredibly mindful of the quality and standards of care.
But I would be remiss if I didn't say we are taking a unique approach because nothing is being done to solve the access or supply shortage here.
[00:16:12] Griffin Jones: Well, I was going to ask Dr. Storment that question, but you know, when you say you're taking a unique approach maybe, and maybe we'll have time to talk about that a little bit later, but I want to say Mate isn't the only group that's using advanced providers or OB GYN to do what REIs sometimes do. And. So John, I want to know what, where's the limit to that. And by the way, that has increased. Since I've been in the field in 2015, there were very few people doing that, you know, maybe Dr. Kiltz, Dr. Magarelli, Dr. Amols a couple of others now it's, there's a lot more people using nurse practitioners for retrievals, if their state allows it or, and, or they're bringing in OB GYN on staff because of this bottleneck. So what's the limiting principle, John, where does. Where does it become something that is not within the purview of the care they can provide?
[00:17:05] John Storment: Well I agree with you. I think that, I mean, I have two PAs on staff and both of them have been trained under supervision to do IUI, HSEs and ultrasounds. And so they, they do them when I'm in the office and if there's problems and we're there to back them up. That's done in almost every aspect of every other type of specialty and how you appropriately use either an OB GYN or nurse practitioner or a PA is probably the crux of what we're talking about.
Right now a PA could come in and do a lot of the things that I'm doing, that they could do a short consult. They could do a lot of the things that I've taught her to do. And I don't think that the patient is getting changed as a matter of fact, because she's able to spend more time with the patient. I think the patients perhaps get better care.
Because of the time that she's able to spend with them. But when, when you're talking about the person in charge of the clinic and the head of the ship is in Oklahoma city is Dr. Patel. So he's greeting the patients. He's seeing the new patients they're going through the things. And then, so does that person who doesn't have REI training and to her point about the United States being unique and that they have a fellowship.
This has been a fellowship since 1973. And to say that it's can be watered down to a short course and to teach them how to do that.
[00:18:30] Traci Keen: It can’tbe watered down at all. We're just, there is a bridge here.
[00:18:33] John Storment: Okay, well, let's go back here.
I'm sorry, real quick. There's no bridge. There's no bridge. When the doc in the office is the only one doing the retreat, the retrieval, what happens when he doesn't have experience in putting when you're three millimeters away from the external iliac.
And it's just not as simple that an OB GYN can go to a short course and learn how to do these, and also have the breadth and depth of understanding of reproductive medicine abnormalities. The you asked about the bottleneck. I think that the bottleneck can absolutely be improved by using OB GYN in the capacity that they can be used by using PAs.
I don't have a problem with that. I think that the problem I see is the patients are being deceived. The patients who go into on your website. There is nowhere near anybody saying that the doctor who you'll be seeing is not a board certified REI, but that's deceiving to the patient for her to think that your doctor has the same training as a doctor down the street, or the doctor in New York City, it simply is not true.
[00:19:47] Traci Keen: Well, I guess, you know, my curiosity and this, this could be a slippery slope, I guess, because there are a lot of non board certified REI who, you know, should they be able to, you know, Practicing the same way, the board certified. I think what we're really getting at and I find it a little bit counterproductive to say that we're being deceitful.
We actually believe in creating a lot of transparency. We're not trying to deceive our patients at all. What we are trying to do is educate increase access And I know that you mentioned that our pricing isn't actually lower. But we do a what's called bundled pricing.
So for instance, a lot of times. We're bundling everything together. So all the ultrasounds are included, et cetera, which can be, you know, $700 per ultrasound. So we're just not going to nickel and dime people through. So when they use the calculator on our website, they know exactly what they're going to be paying for the entire service and there are no surprises. So, you know, I won't say that more affordable than every provider out there, but we do try to keep costs in mind and we do try to build in solutions to make this more accessible to more people. And that's really the crux of what we're trying to do. You know, we're actually trying to honor the REI fellowship by ensuring through our model in a way that.
There is a high level quality of care being delivered. There's ongoing education. There are daily touch points. There are highly trained IVF coordinators paired with every clinic. There is a day to day protocol management oversight by the REI. So, you know, for all intents and purposes, I think that we're trying to increase not only access, but also we're trying to standardize and make sure that there's accountability and oversight along the way. And I guess one of my thoughts is, you know, If you think about, if you were to tell people 15 years ago that you would order a car on your phone and then get into a vehicle with a stranger people would've looked at you like you were crazy and now people do it multiple times a day, every day, Uber, I take very seriously the integrity of our programming.
That's why we've actually, you know, very proactively gone out and found people that we find to have incredible reputations in the industry who also believe in what we're doing, because it comes down to responsibility, access, affordability, standardization of care. And we do feel like we can deliver those things via our model.
[00:22:24] Griffin Jones: So I want to zoom into the Uber point for a second, because that ties into a point that I wanted to bring back to John about. The onus of that transparency. So part of the reason why Uber was able to replace taxi cabs at that scale is because both the public and finally, the governing bodies decided that a taxi medallion was not requisite licensure for carrying a passenger safely to another place.
And John, so when you put that onus on them and saying that, you know, Mate's copy on their website is deceptive. I'm not convinced of that because I don't know who the owner is. If I hire an electrician, is it the electrician's job to say we're a journeyman electrician versus. Sure electrician. It's the view of the governing body that says, this is what a journeyman electrician is allowed and able to do.
This is what a master electrician is able to do. So what's in violation with what governing body here?
[00:23:17] John Storment: I said, it's a great question. And it goes to broader things of some way. Traci said earlier, You have a lot of people practicing outside of their specialty and medicine, all you need is an MD behind your name to be able to prescribe.
I don't even have to do a residency in order to prescribe medication. So there, it's not a great system to sort of prove you say, oh, he's a doctor. I mean,, here's an OB GYN in our area who is doing plastic surgery. They're doing breast augmentations and me. And I have friends who have gone to them and I'm like, you know, why are you going there when they're board certified plastic surgeons?
And the answer is, well, I just thought that since they hung a shingle up, that they were, we're assuming board certification. And so you're 100%, right. That there's not a standard to say. You can't practice without board certification. Board certification does indicate that you've reached a higher level of training and high level of your testing.
And some people are grandfathered into that and some people are not. And so there are people who are not board certified who were practicing and they might not become board certified because of their research project or because of some things that are tied to that. But the realm of being board certified does offer the patient information that they did their training.
They took the written exam, they took the oral exam and they passed all the points. The American board of OB GYN say that's important. And so it is unfair to the public for that person to have the same, the impression that plastic surgeon. Who's really an OB GYN is the same as a plastic surgeon who did a plastic surgery fellowship, but this is much the same.
If it were be honest, he would say, look, I've got Mate Fertility, we've got four births are board certified already. On our advisory board, but the person you'll be seeing day to day is a general OB GYN. And if you say that and the patient says, I still want to go to this guy, he's really a nice guy.
He's a good doc. Then go to him just like you can go to the OB GYN for plastic surgery. I mean, but you have to be transparent and that's.
[00:25:33] Traci Keen: I think that we're being quite transparent about what we're doing publicly and You know, we're not hiding anything from anyone. In fact, we're sitting here talking about it right now on, on a podcast that lots of people will listen to, you know, one of the.
[00:25:47] John Storment: The general public can listen Traci.
[00:25:49] Traci Keen: Please let me finish. You know, one of the things that I think is really important to acknowledge that. You know, we're inviting in the REI community. We are trying to embrace on an ongoing and very active basis. The ASRM guidelines we're trying to make sure.
And I think we're doing a pretty good job of it. ASRM itself has issued statements about OB GYNs performing fertility services and. You know, we really do believe in the integrity that you're speaking about. That's why we're inviting the REI community. And we're actually not trying to take a piece of anyone's pie.
We're saying let's bake a bigger pie and let's do it together. We're taking a collaborative approach. So solve the true problem, which is access the, and who loses in the end from not having access to care is the patient. You know, so if this, wait, if this is just truly about the patients, what are we going to do in the fertility industry Dr. Storment? And I'm asking this to you, how would you try to solve the issue of creating more providers that can. In good faith perform these services. And I'm genuinely curious because I feel like we're taking a problem solving approach to a big problem in this country, the world health organization in 2017, declared it a fundamental rights to build a family.
And, you know, we not only have issues with LGBTQ individuals receiving care. There's geographical issues. There are financial issues. And when only 2% of the population is receiving care insurance companies, aren't incentivized to mandate care because so few people are receiving it
[00:27:33] John Storment: So, I'll go to your first question about access to care.
And I think that that's I've thought a lot about this. I've had some discussions with some of the program directors and the problem with only graduating 34, 40 fellows a year is that's clearly the problem. We all agree to that. And I think that the take is that most fellowships, or at least a lot of the larger fellowships have the opportunity to train more than what they're training. One program director said that she's she's puts out, you know, one graduate a year. She has a total of three fellows. She said I had the capacity to have four times that amount, but I don't have the funding for that. So instead of private equity or VC partnering with general OB GYN to, to increase what might be considered a less trained individuals.
Why don't they put their money into partnering with programs, fellowship programs, endow these fellowships with more money so that they can graduate more people. I would love to see more well-trained board certified REI guys out there that come from well-established programs. And it's not easy.
I'm not saying that it's easy, but I think the money when they partner with private equity and VC partners, Our academic institutions and to create more fellowships that are training better people, that's where we're going to get if we went from 40 to 60. And I think you said in a podcast earlier, but I Griffin you said, you know, how do we get to a hundred graduates a year?
And would that solve our problem? And the answer is probably yeah, because it's going to take a long time to do that but.
[00:29:12] Griffin Jones: How long are we gonna wait? Because people have been saying this since Dr. Kiltz started his model however many years ago. And everybody is saying we need more fellows.
We need, like, how long are we gonna wait for this versus before Mate comes in before I let you respond, Traci, I want to, I was surprised to hear you, Traci use private equity and venture capital in the same sentence, doctors do it all the time. But if I were you, I wouldn't because those are two different camps there.
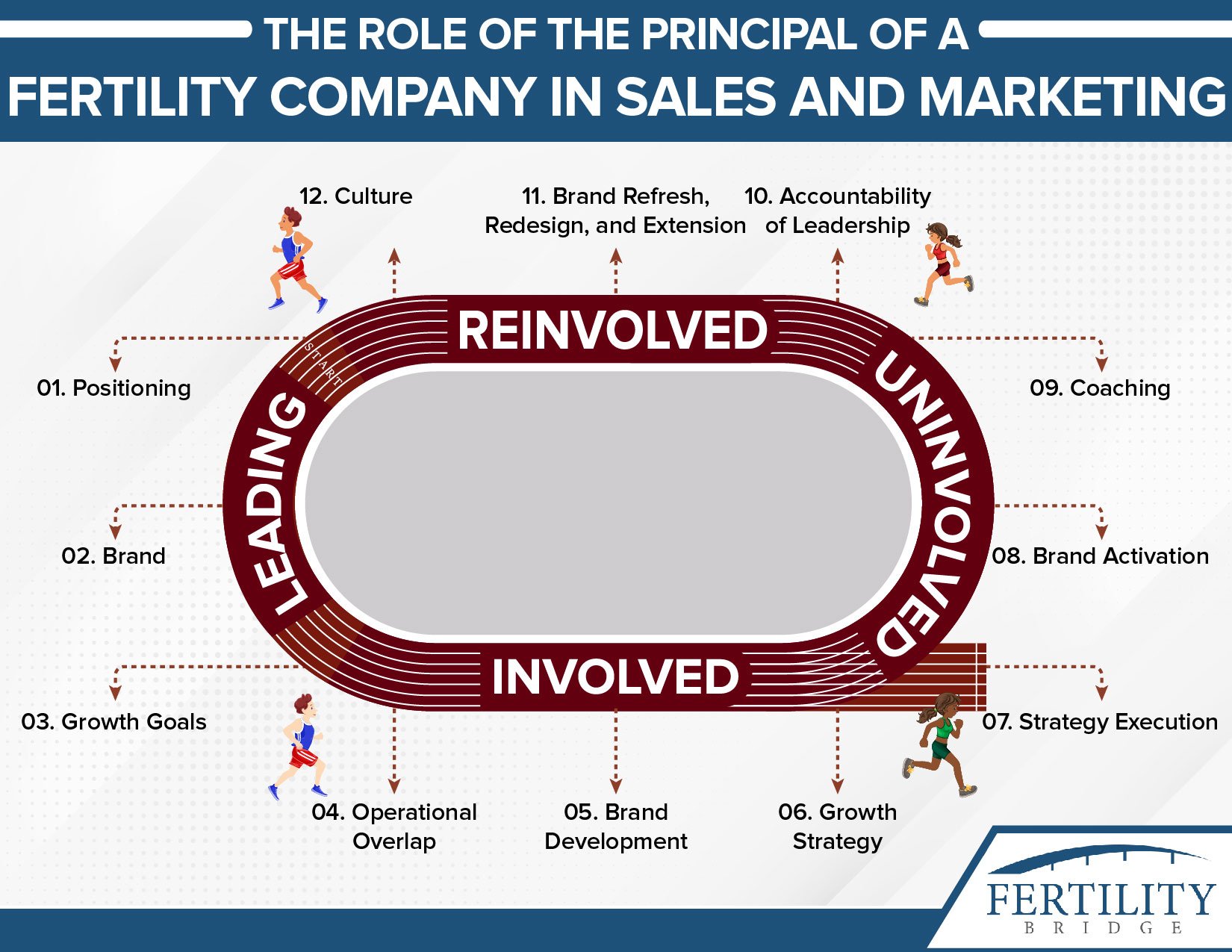
I wouldn't that I don't necessarily want to get in bed with the other. And it's important for people listening. So I'm going to make a distinction because there's a Venn diagram of the two overlap, private equity for the people listening generally coming and purchasing existence. Existing businesses on a multiple EBITDA, increasing profit increasing efficiencies so that they can then sell it up multiple for an exit within a couple of years, usually taking a controlling stake venture capital on the other hand, coming in much earlier stage businesses.
Some that even have haven't even proved a concept yet providing seed funding, letting them get started, usually not taking a controlling stake and. With the idea that they end up scaling into a much larger business. So that would explain why some models would do something and some would others, but all the time, I'm always hearing doctors say venture capital, private equity, very different things.
Know the difference. If you want to see where they come together, watch Shark Tank, because you can act because it's typically a venture play, but sometimes they'll make a private equity play. And so you can actually see where those rings of the Venn diagram. Come come together. And so, oh, I guess like talk a little bit about this, Traci why not the incentive of saying, okay, let's be the ones to make sure that these fellowship programs get off the ground and then funnel that into a different system?
[00:30:58] Traci Keen: Well, you know, I don't know why, you know why not? I think that if that's really, you know, something that Dr. Storment's passionate about, I think he should start pushing for it and create, create that business. Right. You know, it's not our particular model. I think we're taking sort of more of the approach that is taken in other areas and things like where it's almost, you know, we're learning by doing we're teaching by doing.
You know, again, we really are trying to solve for a couple of different things. And one of the things that's important to acknowledge is even if we increase the number of fellows graduating from these programs, generally speaking, they're not going to and we see from the. You know, I think the latest CDC report, if you look at a map of where there's actually fertility care available, there are high concentrations in very specific parts of the country.
And then there are what we call fertility deserts throughout the United States. We look for fertility deserts because just because there's no care, there doesn't mean that no.
[00:31:58] Griffin Jones: But OKC wasn't a fertility desert.
[00:32:00] John Storment: Absolutely not, OKC wasyour first clinic. So why don't you go there?
[00:32:05] Traci Keen: Well, one of the things is if you look at the population density there versus the available care, it's not enough to serve the entire market.
[00:32:14] John Storment: You could've gone to a spot that didn't have anybody. Well, when you have gone to a place that they have two busy clinics and there's a month wait list to get to see any of them right now.
[00:32:23] Traci Keen: Well, you said one of the key words, you know, when we look at markets, if we're seeing long waits. We realized that there's more need than is being provided in that particular geography.
And so we would like to alleviate that, I think as a REI, I think as an REI, you would know that time is of the essence. When you know, when somebody realized.
[00:32:45] John Storment: But Traci, if you have, right now.
[00:32:48] Traci Keen: Storment I would really beg beg of you to sort of you know, the solution of pouring more money into institutions to create more training. I think that that should absolutely happen, but I think there's nothing wrong with trying to solve it the way that we are. I think that we are doing it in line with the guidelines and the the fertility providers. Yeah. I think to say that we're doing something out of compliance with ASRM guidelines would be not accurate.
I think that.
[00:33:18] John Storment: I 100% disagree with that.
[00:33:21] Griffin Jones: Well, let's zoom in. All right. So then John, where are they not in line? Where's Mate Fertility not in line with the ASRM
[00:33:28] John Storment: real quick, I'll get to that, but let's go back. She didn't address the fact that there was a month and a half long. Wait right now, that's not that long for you to see.
So the doctors are either one of the practice. There are a ton of places that don't have REI at all. So why go to.
[00:33:46] Traci Keen: You're trying to go into all of the places that need us. We have to find the right partners in each of those markets. And once we do, we plan to go there, you know, we actually look at the markets a lot differently.
You know, there are certain markets in the United States. Do we want to open them for a Mate, Fertility and LA no, it's saturated. Do we want to open one in New York city? No, we don't. Do we want to open one in Massachusetts? No, they have mandated care. Therefore they're receiving, you know, highest rates in the country 5.5%.
[00:34:18] John Storment: And you guys take an insurance. Are you all insurance plans? Are, y'all not going to take insurance?
[00:34:22] Traci Keen: Currently. We don't, we will provide superbill so that people can submit that to their insurance. And we are trying to facilitate as many points as we can.
As an early stage business, we will evolve.
[00:34:37] John Storment: Well, it seems interesting that you're trying to increase access to care, but you only want it with the cash pay patients
[00:34:41] Traci Keen: what we are trying to create a model that can be replicated.
[00:34:46] John Storment: Why don't you use our model? Why don't you take insurance even on the low paying patients so that you can increase access to the people who have lower paying insurance?
[00:34:57] Traci Keen: I think you, did, end of what I said is that we will, if someone has coverage, we'll provide a superbill for that and the.
[00:35:04] John Storment: That is not, absolutely not covered.
Progeny is not going to allow you to be on there because you're not board certified already out there. There are a host of.
[00:35:16] Griffin Jones: Well, why not Traci? Because it's hard to make an access to care argument. If you're not taking insurance,
[00:35:21] Traci Keen: You know, right now it's just not in our model. We do plan to extend and expand our model.
[00:35:27] John Storment: I love not to take insurance either, because I would love to, to be able to charge you what I want to charge you. The reason why some clinics. You know, $2,000 more than you're charging is because they're not because they're also taking the, you know, Aetna and United healthcare that are paying them $4,000 less than you're charging.
So that's the reason why.
[00:35:48] Traci Keen: We do intend to constantly evolve our model continually, but as an early stage business, Dr. Storment where we're trying to solve for the access issue. And I agree there are problems, you know, but I think.
[00:36:00] John Storment: You are not solving access if you only taking cash pay patients.
[00:36:03] Traci Keen: I think that what would actually be a more curious question again? And I'm trying to look at this macroscopically, not microscopically, you know, I think that attacking people who are trying to create more access, you know, we can go all day about it, but.
[00:36:20] Griffin Jones: I think, and he's making the point that you're not expanding access.
So it's not that he's, Dr. Storment argument is sound then he's not attacking expanding access, he's questioning why you're not expanding access with insurance.
[00:36:34] Traci Keen: Yeah. So what I would say though, is that you know, mandated care would actually expand access more quickly and sometimes things happen in reverse order.
So our thought process is if we increase the number of providers, thus we're increasing the number of treatments. I think that we're more likely to be able to garner the interest for mandated coverage when there's more access, sometimes things work in reverse. Mental health care wasn't mandated coverage until it became more widely acknowledged and accessible.
So we're taking a reverse approach. It may or may not be what everyone agrees is the right approach, but that's the approach that we're taking right now. It doesn't mean that we're not going to continue to evolve our model and eventually potentially take insurance. It's just not something that we're, we're biting off at this time.
[00:37:24] Griffin Jones: Let me remark with regard to the same, I've tabled the, the topic of the ASRM guidelines, because I do want to come back to that, but what you're hitting on Traci is that there's a natural tension between entrepreneurial venture- period, no matter how it's financed-and the practice of medicine. Dr. Francisco Arredondo is going to come back on with his book “MedikalPreneur”. some things I agree with him on some things I don't. I look forward to having him back on, but there is a tension, no matter what people like to say between, and I'm not saying it can't be reconciled ever, but there is a tension between entrepreneurial venture and the practice of medicine in that entrepreneurship prove a concept, fail early reiterate, then build systems to deliver at scale.
And a lot of physicians and clinicians have a problem with that because the practice of medicine is not about that. It's about credentialing, it's about experiment and proven experiment and randomized controlled trials. It's very different. And so, you know, the changing of your model and the changing of many other business models.
It's not this Mate isn't singled out here, but of all of the groups whose model is changing, it's like, you're not the same CEO as the founding CEO. Why not? You have this model for building into OB GYN clinic labs, but you've got to a brick and mortar and OKC. So like, don't you see what the concern is here with with entrepreneurs coming in and having a changing model?
[00:38:44] Traci Keen: Sure. I see what you're saying. But I would say that the only constant in life has changed, and I'm not saying that to be dismissive of the argument, but you know, we can tackle one thing at a time in more successful and add more layers. Do we intend to take insurance eventually? Sure. Do we intend to create access sure.
These are both big goals. You know, when you're looking at a business that's trying to grow and expand and increase access and you're fighting an industry the insurance industry at large, you know, I think the bigger question is why aren't insurance companies covering fertility care. You know, wouldn't that actually facilitate funding of more programming.
There are other things that could happen that would facilitate lots of areas, but we have to be strategic and mindful about how we tackle, when we tackle, what we tackle and, you know, in order to be successful, we can't bite off more than we can chew. If we were to take on 12 things at once and try to solve everything all at once, we would probably fail.
What we're doing is we're taking a relatively linear approach right now that will continually evolve because the nature of a successful businesses typically evolution, you know, I think that what we're trying to do is actually, again, it's a lofty goal, but I don't see it. There are other people I'm sure trying to solve on a smaller scale, but we're really trying to put ourselves out there and again, I would be remiss if I didn't say we're inviting in the REI community, Dr. Storment, you know, if you have ideas as to how we could make this even better, what we're doing, I would welcome your opinion on that and participation, because I think that it's important to look at it holistically and say, who loses in the end?
If we don't start to expand this access. And we can argue all day and night about whether we take insurance or not. And again, I hear the argument, I don't disagree with it. But what I would say is, again, we have to take things one at a time as a business. If we're going to be intelligent about how we approach the problem in the first place.
And I think, you know, we've chosen to go about it the way we are for now, and we will continue to evolve. But again, I would welcome more constructive input as opposed to destructive, because I think destructive really doesn't produce any positive results for this industry at large,
[00:41:07] John Storment: I wouldn't be in destructive and I will tell you that as we discuss this, we keep flossing over the most important part of this.
And that is that you're putting out a non fellowship trained person doing a job. Many would argue, needs to be done at least directly supervised by a fellowship training person. And so it's not the Uber argument. Doesn't hold water because the guys who were driving the cabs don't have three years more training than the Uber drivers were coming in.
I take Uber. I love Uber. I think it's a great concept because what they did is they found a need that the cab drivers weren't doing a good job. And so he said, let's try this, but there's a where it doesn't hold water is you. Can't just say, we want to do what you're doing. We want to take the cash pay patients.
We want to take the simple wins. We'll leave you the really complex ones. And then we're going to just take our money and take those patients.
[00:42:09] Griffin Jones: But cab drivers made the same argument, John, so let's go back to the ASRM guidelines. And so where is Mate Fertility far from the ASRM guidelines in your view?
[00:42:20] John Storment: So there's a ton of ASRM guidelines and you're right. They have, they have made, they have had to make guidelines as to how you incorporate a PA. An NP. And also what's the role of the general OB GYN. They're not about to go out and say something that you can't use general OB GYN in your clinic because of the, of the problem of access.
So they're not going to come out and say, this is illegal, or this is against our guidelines, but they do say that you have to be. Fellowship trained in order to be board certified and the board certification and the fellowship has a whole list of things that we're learning throughout the fellowship.
And these fellowships are not just producing IVF docs. And so I think where they fall short is they're not recognizing the complexity. Of the infertility patient. They're not recognizing that when a patient comes in and she has untreated insulin resistance and she's with the general OB GYN, she might have not have it identified.
She has an egg retrieval. She has suboptimal care and she doesn't get pregnant. Whereas if that person had more specialty training, they would have recognized. That she's a lien PCO that she needs Metformin that she has these other things that go along with her simple complaint of infertility, the patient doesn't know that she has that, but it takes a board certified REI to sort of put together the entire complex endocrine package that she's not, she's not coming with that on her forehead. It's takes a diagnostician and years of experience and a fellowship to identify that I'm not overstating the importance of me because we're great and glorious. I don't, I'm not patting myself on the back.
I'm just simply saying the OB GYN. I don't see a Mate Fertility entering the oncology space to say because there are not enough GYN oncologist, but to try to put a general OB GYN and an oncology space and had to do difficult oncologysurgery or an MFM. That's not happening because it's because that's physically complex surgery and physically complex other things in maternal fetal.
So they're not entering that for a reason they're entering this space because it's low-hanging fruit. And so I think that that's where they, the answer sets up these guidelines, but more importantly, these fellowships for a reason. And it's not just about we want to exclude other people it's it's simply because it takes three years to learn the complexities of reproductive medicine.
[00:44:52] Traci Keen: Well, I would love to ask a couple of questions and, you know, again, I, I approach life and everything with the genuine curiosity. And I do feel like integrity as well. You know, What percentage of the fellowship is academic and what percentage is actual clinical training. And then how much have you had to sort of learn as you go, Dr. Storment and where did you learn that? And how did you learn that as you started your practice, et cetera.
[00:45:22] John Storment: Great question. The structure of the fellowship is for in general, two years of clinical medicine and one year of productive research. And you could argue all day long and I would have left argued to skip the research here because it's just a wasted year.
And I learned after doing a year of research that I learned how to read and write literature. I learned how to interpret the literature so that I can critically look at it and not just look at the conclusion of a study to help better my patients. I didn't like it going through it, but that extra year of research absolutely made me a better doctor.
And when I got out you're 100%, right. I didn't have all the answers. I was absolutely green. And I started with a group with other docs and they absolutely did helped me to go along. And when I got into trouble, they were mentors, but they were in my practice and they were right next door with me. And so doing a practice on your own is tough and being, and not having backup.
So I'm thrilled that you have supervisory roles and people who are board certified. But my fear is that you've had, you have four REI's and one clinic in OKC. When you expand to 10 clinics. I mean, it's going to make it much more difficult to have this daily touch point access to have appropriate backup.
And that's my biggest fear is that patients are not understanding that the doctor is not fellowship trained and they're just assuming their doctor is the same as the one down the street. And when you have decrease the amount of supervision because of how much expansion you're going to make. Then that creates, in my opinion, a difficult.
[00:47:04] Griffin Jones: We only have a couple minutes left.
And there's a question that I want to ask each of you. I have a different question for each of you that I want both of you to answer before. And then I will give each of you the opportunity to close. So For you, Traci is that you do have REIs on the payroll at mate. You know, that the criticism coming from some REI's is that it is business making decisions that clinicians need to make.
Why did you, the CEO, the business person come on and not send one of your REI?
[00:47:33] Traci Keen: I'd be happy to someone in the REI and you know, I'll be happy to facilitate an introduction. You know, I think that one of the things that's important is, you know, while I'm not a clinician, I do value the clinician. And we have a, the way that our model is structured, you know, we try to keep church and state separate for the integrity of the business.
You know, business decisions can't be made by clinicians and vice versa. Because that would sort of make the business fundamentally lacking in the integrity around the choices and the decisions that are made. And I came on the show because, you know, I think it's important that we sort of invite people in, because I think that one of the things that I, I believe in as the leader of this company is if there are naysayers out there about.
Tell me, let help us fix it because the access issue is really what we would like to solve for rather than sort of who's right. Or who's wrong about how it's done. You know, we sort of see our programming as a good solution to increase access. You know, three years ago, I think a lot of people. Less keen on telemedicine in general, you know, and now we've all seen by having to be remote for big chunks of our life.
At this juncture that we can accommodate some efficiencies that way we can facilitate more access unilaterally. And that's what we're really trying to do here is build bridges and increase access. And again, I, I welcome anything that can. You know, I've learned a lot from this conversation and I'm going to take it back and continue to build programming that I think makes sense.
We obviously care very dearly about patients and success and the integrity of the programming and want to continue to build it out to be even better to think that we won't change and get better as we go would be foolish.
[00:49:28] Griffin Jones: Well, John, I want to, and you might want to respond to that, John. And if you do, you can use it for your clothes, but I want to ask you What is the cost of so many areas not having competition?
What does that do to the standard of care? And you're an exception in my view, being in a small market and in some of the markets that you're in, you don't have competition and you have invested a lot in your team building. And what I've constantly said on the show that what used to be business pluses evolves into the standard of care. You know, even referring to mental health providers may have been a plus some years back or having a patient portal. And now online modules like engaged MD or organic conceptions. And, and so like things that used to be maybe like a business or a marketing plus is now part of the standard of care and some of the people that I see in innovating the least in this field are small practices in small markets. And this is not a categorical statement. I want everybody to know, listen it because there are exceptions, but I really see some people that have no fire up under their ass, John. And what does that do?
Because they have this funnel of, you know, 40 plus doctors coming in and none of them in their area. So they have whatever's there. What does that do to the standard of care?
[00:50:46] John Storment: That's a great question. And I'll go back looking at what Traci said earlier, that it is important to want to change.
Being stagnant is not good. I used to practice with a guy who didn't change his protocols no matter what he did the same dose every time. And he didn't do anything different all day long. That's where he did. He did not have a fire under his ass. He didn't care about advertising. He had an ugly office.
There was nothing progressive about his practice and the patients recognize that that's kind of his attention to that. And it reflected poorly. They didn't feel special. And so showing them that you care, making sure that you change and you listen. And sometimes you're right.
Sometimes a Mate Fertility or somebody else moving into your city will cause you to change. And rather than be complacent, complacency is not good for patient care. It's not going to increase access and you can't just keep going along. And we have to have a fire under our ass and our specialty to recognize that access to care is a huge problem.
And as long as we can continue to not do anything about it and not have increased fellowships and fellowship training people. This is not going to be the only model male fertility will be duplicated and triplicated and people are going to be coming in. They're not going to be the only ones doing it.
So we have to be proactive and prideful of what we've created and not be stagnant. And so to that end, that might be an impetus for change. My contention is change and providing a lesser care. And I'm not saying may fertility providing lesser care. I'm just saying you can change. And it can make things worse than what it is now.
And that's why I'm on this program today, because I don't want the care that these people are receiving to be suboptimal.
[00:52:40] Griffin Jones: Anything else that you want to close out your points and then we'll turn it over to Traci to close out her points.
[00:52:45] John Storment: I mean, I love my job and I think the best job. I love my specialty and I'm not this old guy saying I hate change.
I love change. I love that we're embracing the LGBTQ plus community. I mean, probably 15% of my patients, or I remember that and I'm in south Louisiana, so that's fairly progressive. I love change, but I am, and I'm not inherently opposed to private equity or venture capital. Being inherently involved in healthcare and I'm not using them synonymously.
I'm just, I'm not inherently opposed to that. But I think the way to do that is to partnering private equity with academic trainings facilities, and to increase the number of trained RBI's. And I just don't think it's a simple story of Uber and VRBO and healthcare. I think that we're providing care differently than what she's proposing.
And I don't think it will be evident for years. After many couples were realized they were being given treatment by doctors who were not trained as ones down the street.
[00:53:46] Griffin Jones: How'd you like to close out Traci?
[00:53:48] Traci Keen: Sure. I mean, first I'd like to thank Dr. Storment,. You know, I, again, I, I learned something from everyone that I speak with.
And the other thing is, you know, in your last mentioned, you talked about that doctor who hadn't changed his protocol, didn't change it, no matter what the patient is, you know, we view our collaborative model as getting the best and brightest in a room to collaborate on ever evolving industry.
And we invite in anyone who would like to participate and collaborate with us because we feel like there's something to be learned. And if we're all trying to solve for the same thing there's enough room for every. And you know, I don't disagree with anything that Dr. Storment, instead of course, I think that they should be graduating more fellows if they did that originally when the access gap started to widen, mate, fertility probably wouldn't exist.
But we do, you know, feel very passionate about what we're doing. And I know that there are a number of REI is in the field who also feel passionate about increasing that access and solving for it in innovative ways. And so we're trying to do that. While embodying the highest standards of care and also creating a quality control and analysis system so that we're not delivering the same protocol for 30 years that we're evolving with the industry, which again, it's only as old as I am.
So it's going to continue to evolve as everything does.
[00:55:11] Griffin Jones: I would like thank both of you for coming on the show for everybody listening, that's ever listened to an inside reproductive health and a guest of mine says something. And you think that damn comment, come on the show. It's obviously a good forum for discussion Traci Keen, CEO of Mate Fertility, Dr. John Storment and REI managing partner fertility answers in Louisiana. Thank you both very much for coming on the show.
[00:55:35] Traci Keen: Thank you Griffin.
[00:55:36] John Storment: Thanks guys. Thank you, Traci.
[00:55:37] Traci Keen: Bye-bye.