Transcript
Griffin Jones: [00:00:40] On today's show of Inside Reproductive Health. I've got Lisa Duran back with me and we talk about leadership and the struggles that leaders are facing in the fertility field right now - being so insanely busy, crying out for help. We talk about some of the things that they can do and the tools that they need for support. Before I get into today's show with Lisa. I know who I'm going to give today’s shout out to. It’s to Terry and Ed Malanda from Mandell’s Pharmacy. And the reason why is because if you ever hear, when I welcome somebody onto the show and I say, Hey, Dr. Smith, welcome Joe. And I do it in that order. It's partly because of Ed Malanda. I did it like one time and Ed commented that he liked it, that it was the right mix of formal and familiar. And so because of that positive encouragement, that became the tradition for the show. So if you think that super annoying, you've got Ed to blame from it. But today’s shout out is for Ed and Terry at Mandell’s Pharmacy.. Today's show with Lisa is about leadership. We talk about how sometimes there's mutual mystification between partners.
You know what I'm talking about - sometimes there's negativity. People complaining that management level and that seeps through because somebody is allowed to get away with it and talk about change, not being enacted because sometimes it's just a conversation with no follow ups. So we talk about the resources for what leaders need to impact that positive change.
Lisa has been in this field in different corners in solid stints for a while. She was the chief experience officer at Inception. She's been a consultant for the DiJulius Group, she was the chair of the association for reproductive managers, which is how I met her so many different years ago. She's been an individual consultant, so if you want her help, she has that experience and I recommend reaching out. And so I hope you really enjoy this episode with Lisa Duran.
Ms. Duran, Lisa, welcome back to Inside Reproductive Health.
Lisa Duran: [00:02:47] Thank you. I'm so happy to be back.
Griffin Jones: [00:02:49] By the time this airs it’s going to be like episode 114, somewhere around there. And I looked just for giggles of when you were on last, and it was episode 24.
So you were on 90 episodes. It was pretty early on into the show. The audience has grown a lot since then. Overdue to have you back and glad you're here again.
Lisa Duran: [00:03:11] Wow. Well, thanks so much for having me. What an honor it is to be back. And after so many episodes, you clearly are doing something right and something well, so thanks Griffin.
Griffin Jones: [00:03:19] Well, you too, because you had different tenures around the field and not just like a short little stint here, but you've done good yeasts multi-year blocks in different roles as a consultant in house for a clinic at the executive level of a larger company. And so you've gotten into so many different clinics.
You've probably seen the insides of more than I have, and you have also done it in very different business models. So I'm curious as to, if you could even come across commonalities being that some of them are so different. What are some of the biggest challenges that you're seeing leaders face in fertility centers?
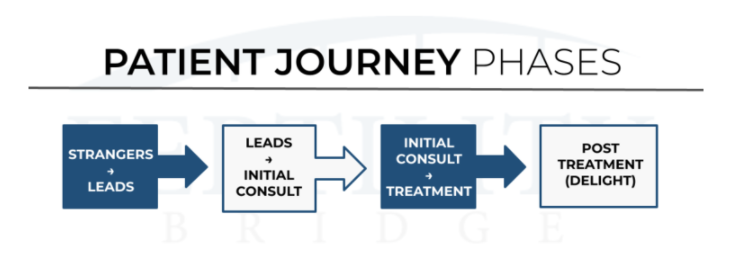
Lisa Duran: [00:04:05] Yeah. That is such a good question. And such an important question that we ask right now. It's interesting because when I started consulting again, I wasn't sure if I would be consulting more on the patient experience side or more on the team member experience side and and the consistent ask is for the leadership experience really, and equipping the leaders because what's happening is that pretty consistently across the board? What an amazing time it is to be in the field of infertility? What we're seeing across the board of course is great. And people are realizing that they want to have a family. And so we're seeing, you know, great growth in the industry and that is, gosh, just such a blessing and such a great thing.
What has happened in the clinics is with great growth, comes different challenges. And you know, the clinics are trying to ramp up their staff. They're trying to hire appropriately. They're trying to onboard and train while navigating, you know, the explosion of growth that they're seeing.
And what we're finding is leaders are just asking to be equipped. Equipped to lead and to go from doing to leading and, you know, the challenges are pretty universal out there. It's navigating the growth. And while keeping, you know, your team morale up and keeping the standard of care where it needs to be.
Griffin Jones: [00:05:26] What are the differences that you're seeing between things that are involved in building the patient experience versus building the team or leadership experience. What are the differences?
Lisa Duran: [00:05:37] Well, you know, certainly in the leadership experience, you know, you're equipping them with leadership skills and we'll talk a little bit about those probably in a little while, you know, you really are trying to influence one to influence the many, right?
And then with patient experience, you know, you’re really pouring into everybody, you know, typically at one time, and then the leaders would follow up, you know, with the standards and coaching and rewarding recognizing, and then coaching for behavioral change. So it's really teaching the skills to the leaders to do all those things.
And I've been really enjoying it. I, most of my consulting lately has really been in leadership and I'm really enjoying it.
Griffin Jones: [00:06:21] What are the skills that they need help with?
Lisa Duran: [00:06:24] Yeah. So pretty universally, there are three things that they are asking for. They're asking to learn how to delegate well. And again, it's going from doing to leading.
That's not an easy transition. So how do they transition that and not make their team feel like they're trying to shove work on them. Right. And we can talk about that a little bit more in a bit, but the second one is coaching for behavioral change because what's happening is they are so afraid of losing good people and losing people because it's hard enough trying to hire the right fit, you know?
So they're so afraid of losing people, what happens is that at times - it’s natural - sometimes we let behavior slide that, that, you know, the behavior that doesn't exactly meet our standards. Sometimes we let it slide or we make allowances or where we give special attention or circumstances, we allow circumstances to dictate what the decisions are and sometimes we'll give people a little bit more. And then you know, and not stick to the standard. And so what happens.
Griffin Jones: [00:07:29] What you just said, Lisa is the reason why there is a crabby office lady or crabby office, man, in so many practices across the world because of what you just said well, but he's really good with the, you know, he's really good with balancing the books. She's really good with billing and or they're the only person that knows this darn EMR as a super user. So we'll let this behavior, I see it all the darn time. And I got to tell you, even as hard as this job market is, we have had some conversations with people that we, you know, we use something called the people analyzer and it's saying like, Hey, this is where you're being rated on. This is where I'm rating you. They give their input and ultimately letting them say, okay, maybe this isn't for me. And even in a hard job market like this, it's been so worth it, even being a bit understaffed because even when you're understaffed, if everybody else feels like everybody else has their back, they're willing to put through the grime of being understaffed. But if you have somebody that even if they're good at the technical aspects of their job, then it's, they're saying, well, why the heck am I going the extra mile? If this person gets away with it, I think that's what you were pointing out.
Lisa Duran: [00:08:53] Yeah, very much. And when there's lack of consistency, on what is okay and what is not, you know, what one person can do versus another and what one person can get away with versus another, that creates resentment. And then with resent, you know, when there's resentment in a team, right, that's not exactly a positive environment.
And then we're asking those teams to deliver a great patient experience. And so that consistency and adhering to the standards and making sure that you're not giving special allowances to people because you're afraid of losing them. So that coaching for behavior change in a very positive way is very important.
And you, people will respect the leader more. And when you know what's expected of you and that's very clear it, people perform better, right?
Griffin Jones: [00:09:39] I want to zoom into the delegating part of that, you mentioned, what trouble are they having with delegation?
Lisa Duran: [00:09:45] Yeah. So, you know, the biggest thing with delegating is first of all, the stigma and delegating people think that delegating is pawning off my work to somebody right. And then, so that, you know, it's letting go of responsibility, it's assigning work and forgetting about it and so.
Griffin Jones: [00:10:01] For some people, it is some people that's it. That's an earned stereotype.
Lisa Duran: [00:10:08] Yeah. I have to tell you that. Being in the centers and being with the leaders, there is not a group of harder working individuals that truly have a heart, not only for their patients, but for their teams and their heart is to keep morale up. Their heart is to deliver a great patient experience. Their intentions are in the right place and they want to learn how to lead. And this is part of it. And they're so afraid to delegate because they don't want their teams to feel like they're giving them more work when they're already feeling a little overwhelmed and you know, so that's really the heart of it. And so it's really changing the mindset that really delegation is sharing work and it's really sharing authority, which can be very exciting to somebody. Who's possibly, you know, who has thoughts and ideas on things or who may want to move up, it's sharing that authority.
And it's also providing team development, right? What a great opportunity to pour into people and develop and raise up that, you know, that next leader. And so it's really changing the mindset and then giving them tools on how to do that.
Griffin Jones: [00:11:15] Where are they getting caught up then? Is it that? Well, my team's already overworked and I just don't want to add more to them, is that the only place they're getting hung up? Where else?
Lisa Duran: [00:11:25] That there's a, yeah, that's a great question. Another place is that they're afraid to give it to them because they are fearful that if that person drops the ball, it's going to affect patient care and that's a valid concern, but done in the right way.
Yeah. With, you know, checking it as a leader checks in on the progress and making sure that before it's, you know, delivered that things are going in the right direction. It won't go there, but that's a big fear they have, you know, “I know how to do it, I can do it”. Right. You know, and I don't know that this person can do it like I can do it. You know, they all have such high expectations and standards for themselves. And that's why they're in leadership positions.
Griffin Jones: [00:12:05] Sounds like that might be in the tool set that they need. What are the tools that they need to delegate?
Lisa Duran: [00:12:11] Well, and I actually take them through some very simple steps that helps them to do that and it would certainly identify the things that you need to let go of and making sure that they're getting the commitment and the buy-in from the team member, but teaching them the process, sitting down with them, you know, a 10 to 15 minute conversation of teaching them the processes, if they need to learn it will be beneficial in the long run.
And so teaching them the process and then having regular check-ins is essential to making sure that again, that it's not going to affect the outcome and accountability. And then also it's an opportunity to encourage that person you're delegating with and, you know, give them encouragement and that they're really doing well and that's, and the teams need that right now.
Griffin Jones: [00:13:02] How often is it that you see positions not having outcomes because I can't speak to the rest of the clinic, but at least in the marketing sales biz dev side, I'm so often seeing no outcome for the position. I think that's a problem. I wrote an article called should I fire my fertility center’s marketing director.
So if you're looking for outcomes, I break it down at each level of marketing. This is what this marketing role can be responsible for. In outcomes because I'm seldom seeing these are the outcomes that I'm expected to fulfill as a marker, which makes delegation a lot harder. Is that how common is that in the rest of the practice?
Lisa Duran: [00:13:43] You know, it really just depends on what they're delegating, you know, they can deligate, things from patient care to administrative tasks. And that is, and that's part of what I teach them is how to discern what to delegate and how you discern that is really knowing that team member that you're delegating to knowing their strengths.
Knowing their sweet spot, understanding are they detailed, are the big picture, right? Are they thinkers? Are they feelers? You know, really knowing them and discerning what you can and can't delegate to. So yes, if you delegate, you know, something very administrative and detailed to somebody, who's a big picture person, the outcomes aren't going to be there and it's going to backfire right and so, that happens.
Griffin Jones: [00:14:26] It happens all the time on the marketing side, where people are given responsibilities and in the practice owner's mind, they're thinking I want profits to increase by X, but the person has no authority over influencing X.
They are given a responsibility or a set of responsibilities that may or may not contribute to X. At all, but they probably do partly, but there are probably other things that are necessary to actually influence the outcome, but their responsibilities are, if not entirely divorced from. They're not entirely unified with those outcomes.
And so can you talk a little bit about the relationship between outcome and authority to affect the outcome?
Lisa Duran: [00:15:16] Yeah, well, and again, that goes back to the responsibility of that goes back to the leader and being very clear on expectations and getting mutual, understanding on expectations and those constant check-ins.
If those check-ins aren't happening, if it's not going the direction that it should have, you will see it along the way. If you're not checking in then and, and the outcome doesn't happen, right the way you expected it to really, it's kind of a shame on you. You haven't checked in and making sure that, you know, the needle was pointing up or, you know, things were moving along the way they should have been moving.
And then you know, As you work with that person and can trust that person more, the check-ins become less and less, but that's essential and making sure that the outcomes are exactly what you are expecting and making sure that the person is very clear on the outcomes.
Griffin Jones: [00:16:06] I think that's a huge reason for, well, just a lot of conflict between leaders is one, the outcome isn't spelled out too, even when it is the person doesn't necessarily have the ability to impact it. And you have to give somebody that seat to own that outcome.
Lisa Duran: [00:16:26] That's right. They've got to have the authority, but you know, it's I think when I talking about delegating probably more in the centers probably it's more of those things that a leader can let go of more probably administrative things. Those things that, that really. Bog them down and stop them from being able to give them the bandwidth to lead and to develop, and rather than big outcomes of whether it be profitability or whether it be patient retention or things like that. You know, that's a whole different level of delegation and right now, these leaders are just are trying to function. They're trying to do so they're trying to be nurses and they're trying to be patient services, you know, advocates. And they're trying to, because they're still doing that as well. And they're trying to lead people and they're trying to hire and onboard and all those things, so really the delegation the tasks that we talk about are probably smaller projects that we'll just take some things off their plate that will allow them some bandwidth.
Griffin Jones: [00:17:30] Do you find that resistance or if not resistance, just difficulty to delegate is more acute where it's an independent practice owner versus a group that is within a large network that supposedly, maybe does or does not have a lot of the corporate support?
What's the difference in the ability to delegate between those two different profiles?
Lisa Duran: [00:17:58] Gosh, you know, that's another really great question. I, as you were saying that, I was thinking about that there really isn't a big network versus a single or practice or one practice owner,there really isn't a consistent I guess pattern, if you will or strength, if you will.
I think it really depends on the leader. You know, there are some leaders that are doers and really just have a hard time prying their hands off things, you know, whether they be in a network or in a smaller practice. And there are others that, you know, that are like, yes, come and help me and so it really just depends.
It really depends on the leader. It's not necessarily. A large network with maybe more support, more corporate support versus the smaller practices. It's really very individual.
Griffin Jones: [00:18:42] So with those leaders, and I was thinking about what you said is that sometimes they may be smaller projects, but I think maybe sometimes they're not smaller projects.
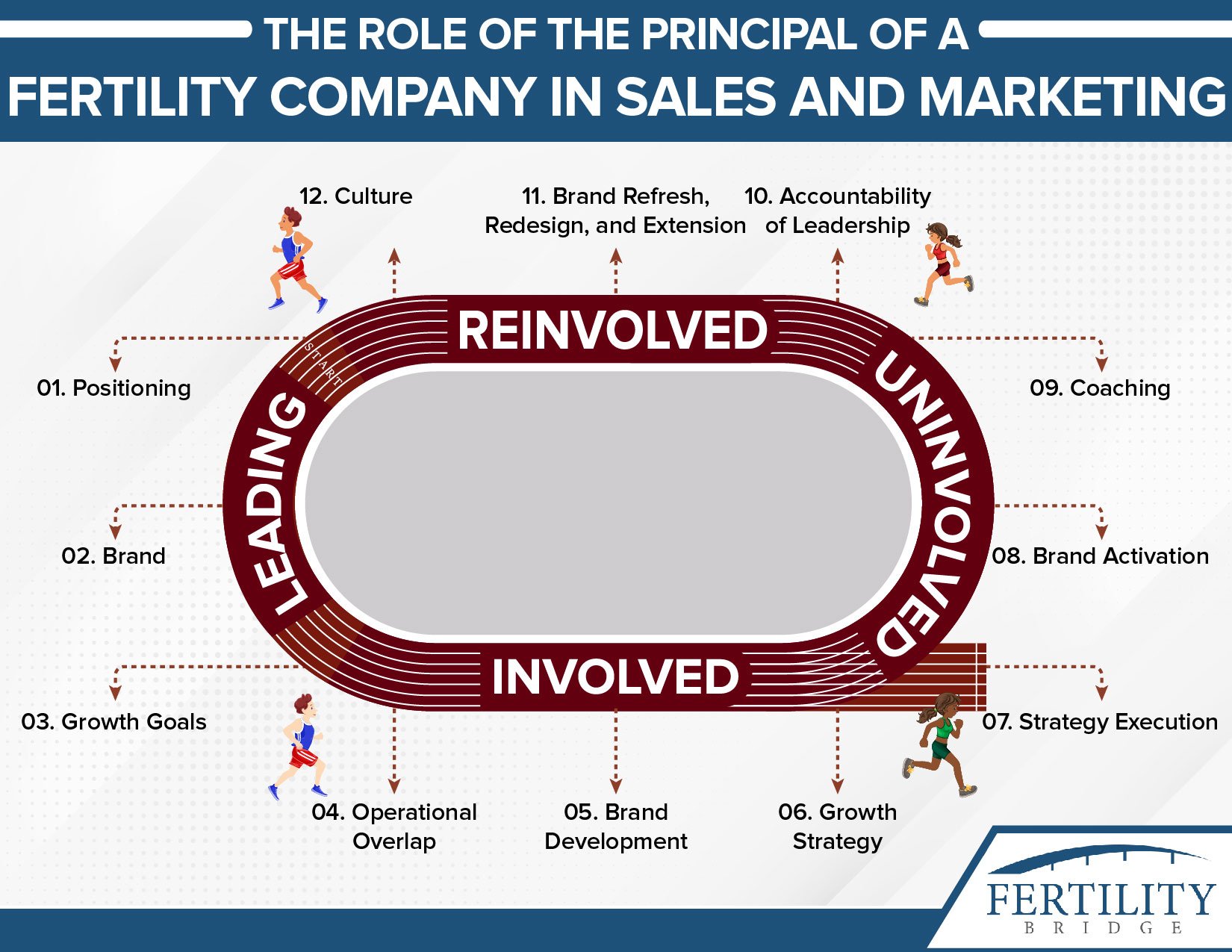
I try to write about where I really, think someone can walk away and where a leader can not walk away. Example in marketing is that I do not believe that the principal of a company can walk away from positioning Fertility Bridges positioning is set by Griffin Jones and I can bring it down to a level that my creative director then makes the brand guide with me.
And then beyond that, I can move out of some of the some of the things, but the positioning has to be set by the principal. That's an example in marketing. How do you help people determine where the leader must be involved versus what they can delegate?
Lisa Duran: [00:19:34] Again, it's really, it's helping them to discern what the desired outcome is and knowing the people, knowing what they can delegate, you know what they can delegate into who, you know, the teams are. So yeah, every team is so different, you know, you walk into a practice and you've got a leader that's been there 20 years that, you know, does this in her sleep. And she's got a team of people that she can delegate those bigger projects to and be very confident in the outcome.
And then you've got a leader that is a new leader. That's really, frankly, is just buried in trying to, to keep their head above water and trying to function. And so, you know, it's, again, it's very individual and just really teaching them discernment that is so big on what the one with the desired outcome is and then and then two who they can delegate to. So, but, you know.
Griffin Jones: [00:20:26] It's a vicious cycle, aren't it?
Lisa Duran: [00:20:27] Yeah, it really is.
Griffin Jones: [00:20:29] If, when your time is so consumed, it is so difficult to step away to actually do the things that the leader needs to do like, you know, when we are in between hiring for positions, guess who's back in helping out in that creative director role Griff guess who's back into the senior digital role sometimes at least for parts of the things.
And that prevents me from building out more of the things that's just part of. Building a business. It's two steps forward. One step back, you get yourself back together and you keep moving forward as a leader. But it really is a vicious cycle that I think many people, I don't know if they've attempted to escape it.
My whole career is about attempting to escape that so that I can build these systems so that other people can do them. But if you can't, if you can't step away to be a leader, then you can't. To delegate those things, which in turn fulfills the prophecy.
Lisa Duran: [00:21:27] Right it's the prophecy. Well, and you know, typically you would say you've gotta be okay to let some things fail.
Right because that's where the learning happens and that's where the accountability comes. And that is really where, you know, again, where the growth happens. And what's challenging in infertility is those, if some of those fails are results in patient care, of dropping the ball on patient care, right, that's not okay. And that's not okay with the leader. And that's exactly what I find is that leaders are so afraid and rightfully so that tells you, you know, about their heart, know, they really want patients to be well taken care of that. They're not willing to risk a patient, not being taken care of with the standard of care that they're wanting them to, or that they need to, right? And that their practice promises.
And so that is exactly why, you know, when you start to delegate, you delegate those projects that are not necessarily going to affect directly. Patient, perhaps it's something, you know, in the process of patient care, but it's not necessarily directly you know, the fail is not affecting a patient, you know, communication or care that and so those are the things that we talk about.
But one of my favorite things to do is when I'm working with like, I do a pre-assessment. I asked him, what are the pain points? Where are the, tell me some of the tasks that really prohibit you from giving you bandwidth to lead. And then when I go in, I'll ask them to identify someone and together. We will sit there and we will go through the conversation of delegating that task and we will do it together. And so that she, or he can watch it in action and feel good about it. And then I will follow up with them. And how did that go? What results are you seeing? Are you doing your check-ins and things like that?
And I'm telling you when they see the results of that, and when they see, you know, how much they can start to let go and when they start to see the growth of their team and how it just really made people feel valued it's powerful.
Griffin Jones: [00:23:24] So you've got an assessment that helps people to measure them.
How else can we help leaders during this time of growth?
Lisa Duran: [00:23:31] Yes. So, you know, the second thing that I was talking about is that coaching for behavioral change. And so, yes, so I teach them, you know, how do you coach for behavioral change? How do you turn that around in a positive way, but yet holding them accountable and keeping consistency in what you expect from everybody.
So that's and that is a skill that is good in life. Right. And especially in leadership if you expect the phone to be answered like this, if it's not answered like that, right. It needs to be a quick one minute coaching you know, a redirect and making sure that the person understands the standard.
They've got their commitment, they've got the tools they need, and that they know that, you know, people don't do what organizations expect they do. What's paid attention to. And also that one minute coaching right away, all the way. Really powerful. And so that's the second tool that I teach them.
Griffin Jones: [00:24:23] That's something that you taught me six years ago, that I still think about people pay attention to what their managers pay attention to. And absolutely true for my team. If I'm not paying attention to it at a high level, it will go away. And if I'm firmly paying attention to it, then they are definitely making sure it gets done.
But some of that sounded like procedural change. When I first, when we were exchanging notes and we were talking about behavioral change, I was thinking skeptically to what degree is that even possible to change someone's behavior. So can you talk a little bit more about behavioral change? Because I often find, maybe it's, I don't know if that what evidence supports or is it against my presupposition? That many personalities are not so malleable.
Lisa Duran: [00:25:10] Yeah. Well, you know, I think about it, I'm a parent that, you know, my kids are older now, but I think about how different my kids' personalities were and one was very malleable and the other one, you know, really pushed on everything that I, you know, that I tried to direct her on and and you know, I had to be much more intentional with her and I had to be much more diligent on not letting anything go by if I, you know, if I expected. You know, a tasks to be done and I didn't follow through with it. It's my fault again, that it didn't get done. And so I don't believe that the people can't change their behavior.
I think that there's, you know, there are two reasons why people complain and there are two reasons why people's behavior don't change typically why it doesn't change and that's, you know, they don't want to, or they don't know how to, it's just become. Right. And so, you know, so figuring that out now that I don't want to, and digging in the heels, that's not acceptable in a business and especially in a business of care.
And so that person should not be on your team. That person should not be working in a company. Right. And but the one that just doesn't know how to, or the one that's been allowed to get away with it for so long that it's just become habit or there's no consequence to it. That's changeable.
Griffin Jones: [00:26:28] I remember you saying your daughter was a J on the Myers-Briggs J which means, which is judger on the Myers-Briggs scale, which means which, and I know because I'm a hard J which means like, we like a plan and that's a different index than like the detail.
I don't need a detailed level of planning. But if I, you know, if I'm making plans with somebody, I'll see you next Thursday at here at seven o'clock, you don't need to send me a text reminder. I'm going there at seven o'clock. And if something changes, you better let me know so I can adjust my whole schedule. And so that's something that you mentioned that you learned about your daughter, and I think that's what you're using for behavioral change.
How much are personality tests involved in the assessment? Are you using it for this purpose?
Lisa Duran: [00:29:45] Very much, absolutely in everything. Absolutely. You know, that, that is such a great tool of Myers-Briggs is such a great tool for teaching communication skills. Right. And for teaching understanding, and being able to delegate based on strengths and certainly in coaching for behavioral change, because if you know, you've got a J or a P, or if, you know, where you have to be a little firmer or, you know, where you can be a little bit more lenient or a little bit more broad.
And so, yes, those every clinic I go to, we start with those, we with those perspectives.
Griffin Jones: [00:30:18] I think I talked about it in episode 24. So, but people probably haven't listened to it in a while. And just liked the story so much that I've got to say it again, but there was a year at, oh, it was at ASRM or something and you separated the group into two and you said, all right, all my big picture folks, if you described yourself as big picture, go over here.
If you described yourself as really detail oriented, go over here and then. Picture. And it was like a picture of Christmas and all of the big picture people were asked to describe it. And we said things like it's a snowy winter's night and Christmas. And someone is finally come home to, to lie against the fireplace.
And the rest of the group was like, there are 12 candles, there are four rings on the rugs. There are three logs in the fire. And I was like, oh my gosh, they really do see the world differently than we did. Yeah. Talk about that with regard to behavioral change, to getting people to use to see, okay, this is how this personality profile might need to receive communication.
Talk about that with regard to behavioral change, to getting people to use to see, okay, this is how this personality profile might need to receive communication.
Lisa Duran: [00:34:09] Well, and again, it's, you know, leadership, I love quoting Spider-Man or a leadership with great power comes great responsibility. There's a responsibility as a leader to know your people and to know their strengths and to ask them, listen, are you detailed?
Are you big picture? You know, do you, or do you make decisions based on thinking or do you make decisions based on feeling so they can adapt their coaching if they don't already know. But it plays a big part in how you coach and it plays a big part in how the person receives it, most definitely.
I recently did a different exercise as it relates to communication with Myers-Briggs and it was the best one. And I thought I'm going to do this everywhere. I go now, where where separated the judgers and separated the perceivers so that remember the judges as, you know, want to make a plan and stick to it.
And that they typically yes, they're more organized and more structured where the peas are a little bit more spontaneous and typically a little bit more on big picture, but much more spontaneous. And I had each of the groups, they had to create a poster of a party invite, but they had to create the poster in the other person's language.
So the Js had to do a poster that would appeal to the Ps. And the peace had to do a poster that appealed to the J's. And it was so great because the J's poster was like, Party starts whenever, ends whenever, you know, food is going to be great. We're going to swim sometime, you know, and you know, and we're going to have a guest, we're going to have a guest, a celebrity guest, and then the Ps how they made the Js invitation, the Js invitation was party starts at seven ends at 12, right? And here's the schedule 7 0 5. We mingle and we have cocktails. I mean, they went all the way through the schedule and at the very end, you know, 11:30 Ubers come and pick you up. And it was just such an eye-opening experience for the way people communicate differently and how they receive communication.
And that it, you know, again and as leaders, it's our responsibility to understand that with our teams. So that's part of this coaching.
Griffin Jones: [00:36:12] It's funny because I described myself as well. I am a big picture person and I'm also a J because I like to know when things are, because I want to move things around, but it sounds to me like the P’s poster would be more or it'd be more interesting to me. Or, I don't know, but I know with Myers-Briggs either you take these four different combinations and then you ultimately end up with four times four, you have six, 16 different profiles and it's pretty remarkable how. When you have yours, that it really gets you, you know, one of the things that mindset is I do like to I sometimes get discouraged if I feel like I'm pushing people, because one of the talents that I have is I'm a motivator, but also I have found in my life that it’s sometimes led me to try to get people riled up about things that they don't really give a crap about. And so, and I'd sometimes get like, emotional about that, of like, well, why don't you want to conquer this? And so really strongly that profile hit me. How do you walk people through their profile.
Lisa Duran: [00:37:22] Well, I deal with the entire team so I always do it with the entire team, including the doctors. That's, it's so much fun and to really be able to dialogue communication styles. And I hope we get to talk about physician support in this too, because that's really key in a lot of this and what's happening throughout the industry.
But I do it in the entire group. The ideal is get the entire team together and we do the profiles together and, and I have the table share their profiles, and then we take some common profiles and we stand up and we really. Then we dialogue them and then we do some you know, some different activities based on what some of the objectives are for that day but it's powerful.
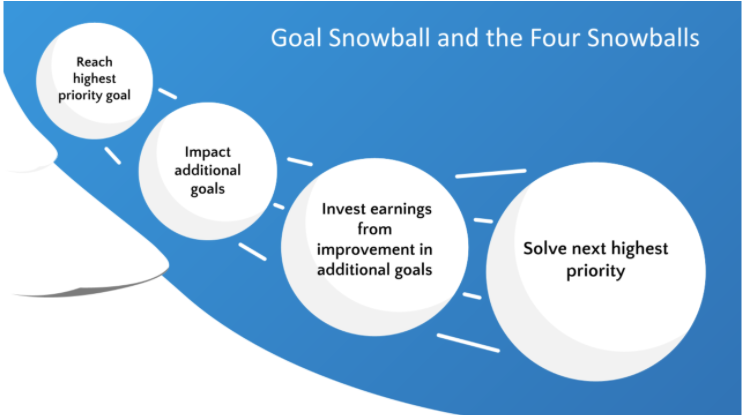
Griffin Jones: [00:37:58] That personality finding might've been the reason that I started the goal diagnostic. Cause I was like, I just want to find out. Off the bat. Do I care about this person's problem more than they do? Because if I do, I'm not moving forward. If they don't care enough about it at this tiny little level, then I am not investing a darn thing left and it's been super helpful, it allowed me to totally emotionally divorced from that and run a much more profitable and well organized business.
But so you're doing this with the teams. You wanted to talk about the lessons and support, and I think I'm gonna set you up for that subtopic with a bit of a loaded question. When you were saying with great power comes great responsibility, a saying that I have is, ”the fish rots from the head”. So I wanted to ask where you see the most, where at what points of the leadership chain you’re seeing the most help.
But my view is that if it's not coming from the top. There's no hope so can you speak to that a little bit?
Lisa Duran: [00:39:06] Yeah. And I'd like to touch on one thing before I speak to that, because it really feeds right into it, you know the which was the third thing that people are asking for, and it's positively navigating negativity in the workplace.
And you know, what happens is when everybody's busy, everybody gets, you know, of short and negativity happens. And then the physician is frustrated because, you know, they're sending attitude and, but yet the teams are frustrated because they're being asked to do things 5 billion, different ways.
And so that, you know, it kind of goes hand in hand, but I'm going to speak to the positively negative navigating negativity first. And then I'll answer the question on the physicians, because again, it really ties in,you know, I talked about earlier how there, you know, there are two reasons why people complain.
This is from the John Gordon book, the no complaining role, it's I absolutely love it. And he talks about how, you know, people complain because they feel helpless, hopeless, like things aren't going to change or it's become habit. And so, so I absolutely love whether it be with leaders or teams. And we talk about that and I have them write down all the things that you complain about, you know, no one's going to see it.
I give them little journals, write down all, everything you complained about. And then John, in his book, he goes through three steps and how to turn a habit or a mindset. And do you know how to change that just with very simple steps. And and so, you know, first of all, teaching the team, that concept, and then teaching the leaders, how to expect that from them and how to condition them.
You know, one of my favorite quotes from the book is complaining is like vomit. You feel better afterwards, but everyone else around you feels sick right and isn't that the truth.
Griffin Jones: [00:40:52] A hundred percent and it spreads and it's very common in office environments. It might be even more common in, healthcare office environment.
So how do, so what, how do we support the physician in a way that?
Lisa Duran: [00:41:09] Yes. And so what I found I've actually had some really amazing meetings with some physicians where they've, you know, I've had one on ones where they've said, gosh, I don't know what I'm doing wrong, but I feel like I'm complaining or I'm yelling at them all the time because they're not doing things.
And you know, my, because I'm a pleaser my first reaction is like, oh no, Fine. But I have found myself in, in, in these years, the older I get, I guess the more season I get, I find myself a little bit more bold you I, you I tell them, I said, you know what? You are such an amazing physician because you do things the way you do them.
And you putting your personality into your spin, you know, fighting for what you feel is right. Whether it be a process or a protocol or a delivery, whatever it may be, and I need you to understand what that does to the team, you know, can you imagine, I tell them, can you imagine starting a new job and saying, this is how you schedule an appointment and then you have four different physicians saying my patients, this is how it's done.
And you have four different ways of things and then you wonder why three months later, that person leaves and you're frustrated because now the ball's being dropped because your patients are being taken care of it's because there are, these teams are having to navigate not only how to, how to do everything and how to, how to give a great experience, how to give great care, but they're learning how to navigate different processes with each doctor.
And especially in those larger clinics, it is so challenging. I feel so bad, you know, I keep thinking, you would never hire me on patient services because you would fire me. I don't know that I could remember how everybody wants to do, how differently everybody wants to do it. So, I tell them you've got to let go of some stuff and, and, and the team of doctors need to come together and you guys need to try and create some continuity.
What are some things that you can let go of to create some consistency, to help the teams out? That's how you can support them.
Griffin Jones: [00:43:10] But that's a leadership issue in and of itself, iIsn't it of having, this is my way. This is our way. That's not a united kingdom. That is a different section of fiefdoms controlled by different warlords that allied together sometimes for certain resources that is not a United front.
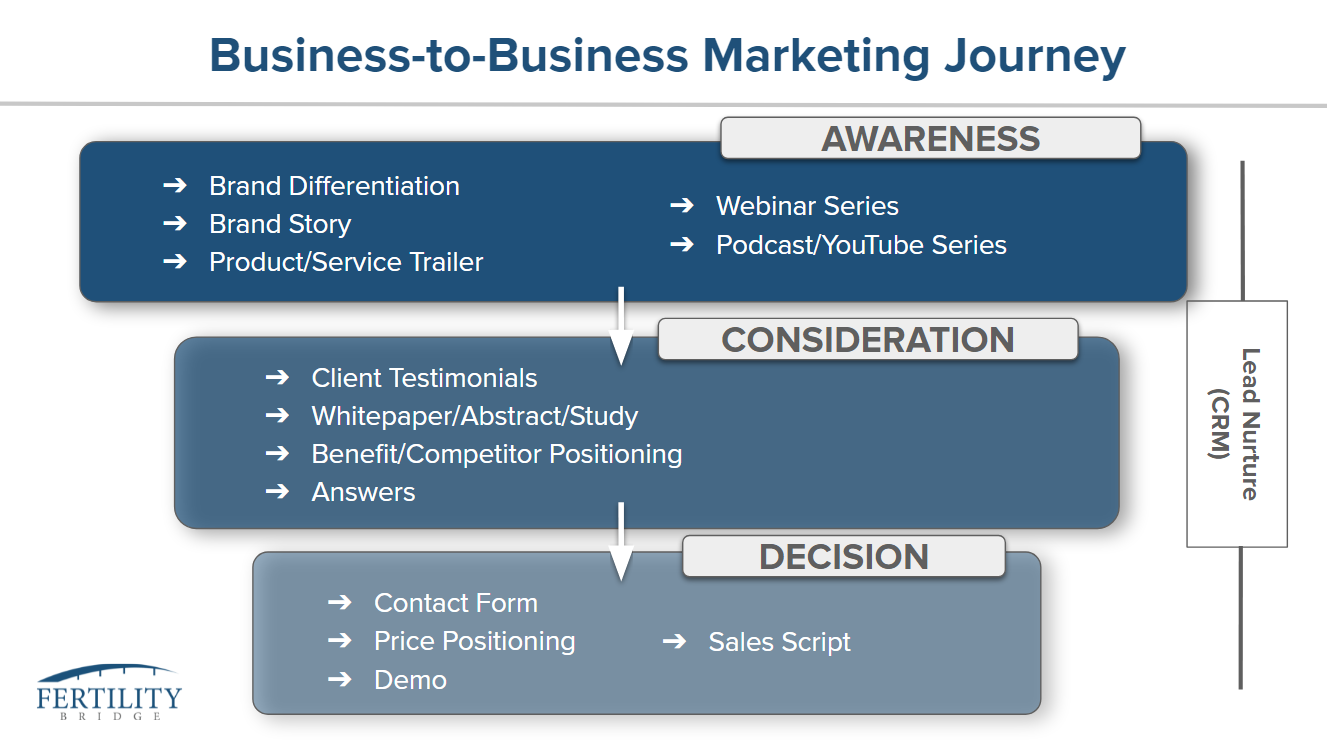
That's where I really push people when I've had people like Dr. Eckstein on the show and I'm pushing people. And I'm saying like, how do you rule by committee and consensus? And there's some people that have good and like Dr. Washington has good thoughts on that, but I really am just skeptical of the whole thing. It's part again with like this little gold diagnostic thing that we do, what we're doing in the very beginning is can we get all of these people on the same page in the beginning? Because what I used to find, when we would get into agreements with people, we would find out three months, four months, That the other partner is a totally different idea and it would just,lik, throw a wrench in works and what the hell man.
Like if you're not successful, I'm not successful. And that affects my reputation. And so, that was an issue of leadership. It's like, okay, we have to get people in the same damn room talking about the shame. Damn.
How do you get that united front?
Lisa Duran: [00:44:30] You know? So to be honest with you, Griffin. I I have just barely started having these conversations with physicians, but I will tell you that I'm dying to have them have me back because I, you know, I tell them, I'm like, look, you know what I will facilitate, you know, let's get the four of you in a room, let's first identify before we do that, let's get the team together and identify the top three things that are very inconsistent with all of you. And where consistency will make a huge impact. Once those are identified, then get the four of you in a room and let's look at those processes or those protocols and figure out where you can create some consistency, but having someone facilitate that again The out the objective being to make the lives easier for everyone to lessen their frustration as physicians and to, you know, for team retention.
So we're not turning our teams so much. And you know, in boosting them around and also having less things to have to be frustrated with them about, you know, let's do that together. And I've had a lot of, you know, a lot of physicians say, that's great. I'm willing to do that again. It's just, let's do it.
Right. Let's do it. Let's take that step now. It's going to be just a little, you know, I mean, that's it's a huge issue. Right? And so I'm not claiming that I, you know, that I can even begin to try to fix it, but I figured, you know, what, if we fix, you know, if we can fix three things and create some continuity there, then let's start there.
And then three months from now, let's visit another three, you know, or six months from now, let's visit another three and let's visit another three. And let's just try to make some progress because we've been talking about this for years, right? Right.
Griffin Jones: [00:46:15] Yeah. There's a lot of mutual mystification between part.
I hear it all the time. Like, well, you know, I'm talking about selling to this group or I'm talking about hiring this person, but I don't want to tell Dr yet, because. They own X percent of the company. You might want to bring it up before the last minute. And I think of all the groups that we've worked with, there's been one where we have been like their mediator in this way, but I haven't a hard conversations is a part of leadership, isn't it? Yes. Isn't it like the most important part of leadership, because otherwise you end up leadership is about getting all the boats to row in the same direction. If you can have hard conversations, you can't get the boat rowing in the same direction.
I have a key team member that within the last month or so we had to have an uncomfortable conversation and it was important because there was just a bud of resentment on each of our ends and we're able to nip it in the bud and come to, but if we didn't have that conversation and we had to have two of them, then just that little resentment would have grown more and more. And so how.
Lisa Duran: [00:47:29] And that is exactly how it happens.
Griffin Jones: [00:47:30] How do you facilitate the, all I do is just get them in the same room and act like a dick. And they either team up against me or, or realize, oh yeah, maybe we should be doing this, but how do you do it more constructively?
Lisa Duran: [00:47:45] Frankly, to be honest with you, a conversation is not going to do any.
I'm just being transparent with you. You know, we can, I can, you know, bring people into a room and have a conversation with them and say, Hey, you need to line up and you need to be, you know, whatever. Or I wouldn't say that, but I'd facilitate that conversation of how, you know, how are you feeling? How does this make you feel?
But really it's going to be in the action. So, and that's exactly what I'm talking about the, you if, if you've got buy-in to going, okay, let's look at the processes and then you walk away right. Then they don't have time, facilitate that, you know, that exercise and you know, the, again, the practice administrators and the leaders, they're the most hardworking, amazing people, I know, you know, they are trying so hard. And so, so it's really investing the time. It's really investing, you know, a couple hours, you know, every three or every six months. And to not just talk about it and not just get agreement, but, and maybe not even get agreement, but really just talk about it and big and not just talk about it, but figure out the solutions, take a very specific protocol or a process.
And do it right there. And then have it be, you know, when everyone walks out the door, whether you like it or not, you know, some things you’re gonna like some things you're not, and this is how we're going to do it. We've all done. This we've all worked on this together. And so, know, really it's gotta be a lot more than just conversation.
Griffin Jones: [00:49:10] Because that's the solution to one of their two reasons for complaining, which is it's helpless, nothing's ever gonna change, or it's always but the other one has always been this way. That by changing it and reducing that negativity. And when you brought that up, it made me think that my people almost never complain about clients and it's because I almost never complain about clients. And that wasn't the case in the early days, I notice that my team would like, complain about clients a little bit.
And they were getting that from me. It's ‘cause I would make like a snide comment about something. How do they not have this together? And then I zoomed in and realized, well, it's one of two things - either I'm a know it all and I'm not appreciating what somebody else is going through in their business, or we have a saying in our company where there's no such thing as bad clients, there's only bad prospects and bad process. And I had to look at myself and be like, what is it about my process that is allowing these relationships to manifest in that way, and it wasn't easy to fix it. I really had to change how people come into the company, but once they do, like, we have a really good relationship with them and now I'm not complaining anymore, which means my team isn't complaining anymore, which is good because we should not be complaining about our clients who are working their fricking tails off.
But it was something that I had to fix at a fundamental level. So what are those to do's that you're giving people? They can take a while.
Lisa Duran: [00:50:40] Yeah, they really can. And I'll share those to do's with you. But I want to tell you that this was a very personal journey for me as well. And I picked up that book because cOVID really got me in a funk. You know, I'm an extrovert on steroids and I love being in the clinics. And for me to be, you know, in my home office, by myself for 10 hours, I was like in the fetal position, you know, when people and I found myself chronically complaining and it just became habit. And that is not who I am.
And it was really ugly and I began to not like who I was. Right and I'm like, who is that? That's not you. And I love, you know, there's a, there's a saying that I absolutely love, and it says. Of your heart. So your mouth speaks and so, you know, I realized a lot of this was a heart issue and a head issue.
And so when I picked up the book, you know, I was like, okay, I gotta change my heart. And I got changed my head, you know? And so, you know, the hearts, one thing, the head is another. And so what are those tools? So those tools, there were three things, he gives you three things which were so great, number one is you start with the they get two versus the half two instead of I have to do this by five, you know, I get to do this by five, right. Instead of I have to stay home in my home office, well, I get to work from home and you know what I can be in my yoga pants and a t-shirt all day, you know, replacing and changing the mindset. And so you replace half two with get to, and that's a very practical thing.
And so I did the exercise where I wrote down all the things that I typically complain about. And then I crossed out half two and forgot two and so that became, you know, what I did. So step two was racing the butt and doing the and, you know, and not saying something great. And then saying the but right. But this really sucks so this really stinks, you know, replacing them and seeing him saying things like, you know, wow. I'm just, yeah, I've got so many projects right now. You know, and I'm, I'm going to get them done, not, but I don't know how I'm going to get these done. So, you know, again, replacing that and so changing some of the verbiage helped change my mindset, but the third one was the most powerful. And that is the one where there are boundaries set in place that I had to get people on board with me, people that I would talk to all the time. Tsey-Haye, she's a good friend of mine from Inception. I'm gonna tell her, I'm like, you gotta help me keep these boundaries, you know?
And the boundaries, we're you know, you're not allowed to just complain any time. You're not allowed to vomit on me all day long and leaders. And that's why I tell leaders. I said, if you're walking across the floor and you're going to see a patient and you let one of your team members come up and vomit on you about something, and you're going to go see that patient unacceptable, they may not vomit on you while you're, you know, needing to go do something. So, so how do you know when can they, you know, people should be able to complain, but turning complaining into productive solutions. And so, you know, that is the key. So creating the boundaries on how they do it, and we've all heard the don't come to me with a complaint without being part of a solution, but he really breaks it down very nicely.
And really holding people accountable for being part of the solution so one of the things I work on with leaders is how do you actively listen, validate their feelings of their complaint and saying that is, you know, those are some great points. And tell me what ideas do you have to fix this?
And what part are you going to play on this? I want to support you right. And then holding them accountable for that. I'm telling you when you make people be part of the solution, not just say it, but make them be part of the solution. You're good, they're not going to come back and complain to you very much.
Griffin Jones: [00:54:19] Yeah. My operations manager says you have something you want to do at Fertility Bridge, bust out the mirror because that's the person that's going to be doing it. But as you're talking, Lisa I'm seeing the reason of the importance. For this reason as connected to each other, meaning it's so important to not have complaints and be complaint driven only, and to be solutions focused, partly because of how sensitive the self-awareness has to be to improve as a leader. Like the things that you're talking about, I don't have to, I get to - that’s counted all joy. That is a very difficult mindset to get in and there's just so much of a leader where you have to be brutally self-aware about everything that you've built.
It's like everything I’ve built like this still, is that good or this still needs to be improved, this particular part. And because you have to be so introspective. It can feel like salt in the wound when somebody just comes on like, well, why aren't you doing this? And we had somebody, we had a candidate, a job candidate last week that was like, well, why don't you have this type of social media post is like, oh, I don't know, because I'm busy making payroll from a company that I built from. Absolutely nothing. When I called Lisa Duran from a fricking orphanage in 2015, and I'm building all these systems and serving nineteen different clients and building a point of view for everything, because I never took a dime of that's why,
like just as you're talking, I think that they're reciprocal, the solutions orientedness has to be what makes. Wound not stinging so much when you are being introspective enough to actually pursue the change.
Lisa Duran: [00:56:13] No you're so right about that. And it seems overwhelming to a leader, but, you know, I used the example of, you know, you've got, let's say you've got a group of team members that are gossiping or that are complaining about something.
How powerful is it? And, there's kind of a ringleader in it is when a leader takes that person aside in their office privately, and just saying, Hey, listen, I know I heard a lot of that going on. And you know, I know that we all want this to be a great workplace and you know, I know that I trust you and I want you to trust me.
And in order to trust you, I need to know that you're going to have my back on everything. And I want to have your back on that. Let's talk about that, to talk about that hard stuff, but the reward. Yeah, the relationship and the strength of the relationship, the reward, and that the leader walking away going.
I just taught somebody to, you know, to navigate some negativity, to possibly do that. And I just strengthened a relationship. I talked about something really hard and, and I got a partner. Right. And so intentional. It's hard, right but the reward is just so great. And I would just, you know, when people do it and they feel it and they see it's powerful.
Griffin Jones: [00:57:29] You've given us some you've walked us through personality assessments. You've given us the framework for getting leaders on the same page, how to support the leaders so that they can support the next leaders and to delegate. How do you want to conclude with supporting leaders in the fertility field?
Lisa Duran: [00:57:47] You know, my heart really went when I go into a clinic, I just want to grab them and hug them and just say, you're doing amazing. You're doing amazing because again so many of the leaders out there are just really struggling with feeling like they're doing enough. And so, you know, part of, you know, what I love doing is inspiring them and equipping them first, inspiring them to them to know that they're doing enough and then equipping them to do the things that are going to make a difference in, you know, it's going to help give them bandwidth and help their teams just feel so good about, you know, what they're doing.
And so, I, you know, I think that's, I just want to conclude with I'd love to tell leaders out there. You're amazing. And you know, this time, this busy-ness and the craziness of the growth is just so wonderful. And the season will pass. They'll be some low leveling off, or you'll be able to breathe.
But the growth, you know, the hard times don't produce heroes, the hard times bring out the hero in you. And so I think that I love just watching the hero being brought out in people who've, who it's always been in fight of them.
Griffin Jones: [00:59:00] I get to become a hero.
Lisa Duran: [00:59:02] Yes I get to become a hero, that's right.
Griffin Jones: [00:59:03] I get to become a hero. There's probably a lot of people that could use that right now. Thank you so much for coming back on us.
Lisa Duran: [00:59:11] Oh Griffin, thank you for having me. I'm always so honored. I have to tell you, I was talking to a clinic today and I said, I've got to go. I said, I got to quit. I'm on a podcast with Griffin, from Fertility Bridge.
And they're like, oh my gosh, you get to do that. And I was like, yes, I get to do that. So I think you're kind of famous there Griffin so.
Griffin Jones: [00:59:29] There really is full circle. Thanks so much for coming back on, Lisa.
Lisa Duran: [00:59:32] Thank you. Take care.