[00:01:08] Griffin Jones: The first global brand in the reproductive health space. And if you think there's been global brands before listen to this episode, because I'm talking about consumer brand, this is the first global consumer brand in the reproductive health space. It's Kindbody. I've got CEO, Gina Bartasi back on.
After a couple of years, we talk about what Kindbody has been up to in all the markets they're in and where they're going, talking about the history of their acquisition with Vios, they've raised tens of millions of dollars in venture capital funding. There's a couple of things that I pushed back on Gina about talking about this concept of this Jeff Bezos, Amazon Sam Walton, Walmart type of end to end channel domination. They Kindbody is going after. There's a lot that I'm not qualified to examine. I'm not qualified to examine on a lot of their business model and certainly not the clinical side. And I know that a couple of you are going to think that I'm kissing rear end when I'm, when I talk about brand, when I go into that part of the I will fight you. I am not kissing any, but I am telling you the things that I've been telling you for years, and I'm seeing somebody do in practice and now people are starting to feel, oh, this isn't just about bringing new patients in the door. This is what it means. To have a brand that is not window dressing.
If you think that Kindbody’s brand is, oh, that's just good marketing. That's just pretty stuff. It isn't, it's the foundation of everything that they've been able to put together. And it is an extreme, competitive advantage in recruitment and retention of employees among other things. So if you'd like some help with that guest who does that for us?
The firm that sponsors this podcast, of course, Fertility Bridge. And we are helping a lot of different practices across the country to up their brand, regardless of whether they have a patient acquisition challenge or not many of you don't, but there are reasons why this branding and creative messaging really, really benefits groups.
And we talk about that today. So you can tell me if you feel that I was kissing her. If you feel that I was too tough, you let me know, enjoy this episode with Gina Bartasi.
Ms. Bartasi Gina, welcome back to Inside Reproductive Health.
[00:03:40] Gina Bartasi: Thank you. Thanks Griffin. Nice to be with you.
[00:03:43] Griffin Jones: What is it Kindbody been up to in the last two and a half years since we spoke, nothing right?
[00:03:48] Gina Bartasi: Nothing, not anything at all.
[00:03:50] Griffin Jones: Not a damn thing.
[00:03:52] Gina Bartasi: Sitting, twiddling our thumbs, trying to figure out what we're going to do next.
You know, I've always said the success of any businesses, only about its people. And so we have an extraordinary team. The team has parlayed their knowledge and experience into a tremendous amount of growth. Right? So today we have 26 locations not the least of which is the new virus clinics that will pull into the Kindbody network that acquisition closed February 1st.
And then those Vios locations will be rebranded Kindbody. But Angie Beltsos is one of a kind you know, I know that the audience is aware of all the PE money rolling up practices in the industry. We are not a roll up firm. We have preferred to build de novo, but Angie is unique. She is extraordinarily talented as a physician and she is even more talented as a clinical leader, just as a leader in general, she knows a tremendous amount about business, about productivity, about margin.
And so, yeah, we have 26 locations. We'll be adding another 10 this year for 36 locations by the end of the year. And then we're back in the employer business. So we see quite a bit of interest from the employer business. Certainly our consumer audience that we started with is still a big part of our revenue.
And then we see quite a bit of payments come from the managed care industry.
[00:05:15] Griffin Jones: She knows the answer to this, but I don't, is Vios the first acquisition that kind of body is done in terms of presence?
[00:05:21] Gina Bartasi: I noticed the first acquisition, I've done quite a few acquisitions in my career, but it may be the first one at Kindbody.
I shouldn't, it should be an easy answer. We haven't bought any other clinics. I'm trying to think if we've bought anything else, I guess not. So Vios is the first, it will be the last multi-site multi-physician practice we acquire again, we prefer to build de novo. We wouldn't rule out some of.
[00:05:45] Griffin Jones: This podcast lives forever Gina, do really want to say that it will be the last.
[00:05:49] Gina Bartasi: No Griffin, it'll be the last multi-physician multi-site acquisition we make, we may make some tuck-in acquisitions. Right.
[00:05:58] Griffin Jones: But even that, why rule that out?
[00:06:00] Gina Bartasi: Because I know the multi-site physician groups and they are already owned by one of our peers that are not a lot of multi-physician groups, still standing that are independent, there's probably less than 10 in the entire country and the 10.
[00:06:16] Griffin Jones: All multi-position and multi-site meaning multi-site meaning more than one lab. Is that what you mean?
[00:06:22] Gina Bartasi: That is exactly right. That is exactly right, because we wouldn't be interested and it's too easy. Thanks to our extraordinary real estate team for us to stand up a clinic with the lab. They've gotten very proficient at it in the last 12 months. So the reason we would make a multi physician, multi location acquisition is to get scale. There is not, again, there's probably less than 10 of those.
So yes, there are multi-physician, but maybe they only have one lab and then one satellite office, which would rule them out. So that's the reason it's an emphatic statement. I think, you know, we're getting a lot of requests now. From the employer market to think about international expansion and so potentially internationally, we wouldn't rule it out, but in the United States you know, and Angie knows everybody as well.
We are looking for physicians that are like-minded, you know, Angie, she's wildly unique. And so she's amazing, and we have so many other amazing physicians, but there's a culture at Kindbody and Angie believes in that culture, the culture was almost identical to what Vios culture wise. I mean, we prioritize patient care.
The patient always comes first. Our employees come first, you know? And so there was this, this real foundation and we are here to serve others. And so that's what makes, it's one of the things that makes Angie and Vios so unique. And it's also the reason. I think we're limited in terms of other potential acquisition targets is rare to.
So, seamlessly be able to put two companies together that agree on so many things. Usually when you're rolling up things or you're putting two things together, there's a lot of friction. The integration is hard. There's a lot of disagreement. There's a lot of debate about, oh, and you just don't have any of that.
You just don't have any of that. We are incredibly like-minded now we've known each other a decade and that probably helps as well.
[00:08:19] Griffin Jones: Well, I want to ask about how you did that vetting because it sounds, it reminds me a little bit of like the Facebook, Instagram, sorry, where Zuckerberg said you, most of the time, we're not going to do.
Acquisitions most of the time we're going to be building out Facebook property now, meta properties. But at the time they saw something that was perfectly in line with what they were trying to do. They stole Instagram at the time for $2 billion and it totally fit. And so that's what you were describing with the Vios acquisition, but how did you vet it to that point?
[00:08:51] Gina Bartasi: Yeah, again I think knowing Angie and Greg for more than 10 years was extraordinarily beneficial. We had talked on and off for the last several years. Again I've thought Angie was just as unique as I think she is today. I thought that the first time I met her at 10 years ago, I met her at PCRs and she's so articulate.
She listens first, most leaders talk first and listen, second, Angie listens first and talk second. And that's a rare characteristic to be both a leader and an extraordinary listener. A lot of leaders are not as humble as Angie is. Angie is extraordinarily humble. And so I would watch her in meetings.
I would watch her interact. I was like, wow. She is a total bad-ass and I always wanted to work with her. I did work with her. I worked with her at Fertility Authority. I worked with her progeny and as time grew on, the affinity grew more like she, she continued to impress me. And she continued to raise the bar.
I knew her when she was at FCI, I watched her grow Vios she does everything with a tremendous amount of elegance to and class. And that's hard to do. It is really, really hard to scale a business and grow a company that fast and keep your cool and take the high road and work hard and not lose it while you're trying to juggle all these things.
And she just did it, you know, and I watched her. And so anyway.
[00:10:18] Griffin Jones: She does do that by the way. No, I don't talk about things that happen in business meetings on the air, but Dennis, at a super high level, I think Dr. Beltsos is comfortable with me saying she does that. We'll be quiet and let everybody talk and then she's, and then it's like, all right.
And then she's honest, like she lets people say it and you get to see your processing and then boom she's she's got it. So you described her well, so that got you into the Midwest. So you, you found this really good culture fit for you all you acquiring Vios and then, and now you're in the Midwest.
What cities are on the, the docket that you can tell us about now?
[00:10:54] Gina Bartasi: Yeah. Well we want to be completely transparent, so we don't mind sharing with the audience, but we're opening Seattle. We're opening Dallas, Houston, orange county Miami, Charlotte we're opening in Washington DC next week. Two weeks.
May 4th. Whenever that is. Oh, maybe it's in more than two weeks. Maybe it's in three or four weeks. What am I missing? Should be like, we've opened two already. We opened Denver two weeks ago. We'll open Dallas in three weeks. Excuse me, Denver. What did I say? DC? Dallas. Houston. I'm missing some, but anyway, that's kind of the footprint.
Oh, we're opening Brooklyn, a third location in New York. I should have the map in front of me, but that gives you a general idea.
[00:11:35] Griffin Jones: It gives me an idea of the near term is, I mean, in a few years time, are we talking about everywhere? Gina? Is that the play? Like, are we going to see Kindbody Cleveland? Are we gonna see Kindbody Buffalo?
Are we going to see?
[00:11:46] Gina Bartasi: Columbus, we're actually coming to Columbus before we're coming to Cleveland. We are, we're taking and we're adding a location in the east bay. So both New York, San Francisco and LA we'll all have three locations, but I think that's right. Our plan calls for 50 locations within the next two years.
We want to be where our patient population lives and works. The majority of those locations will be retail in nature. We, you know, believe in the consumerism of healthcare and really building a global brand. We talk about a national brand, so our eyes are set on the US over the next 24 months.
But in three to five years, I think you would see con body locations internationally as well.
[00:12:25] Griffin Jones: I want to talk about that global brand and what Kindbody is done to get to what you have now. I am jotting that down because I want to ask you a little bit more, but I don't know if the employer benefits side was part when we spoke a few years back on this show.
And so what has changed in, in employer benefits from, from when you started Fertility Authority and then, and then progeny that or whatever, what was that? Seven years ago or?
[00:12:53] Gina Bartasi: Yeah, seven years ago.
Yeah.
[00:12:55] Griffin Jones: So what has changed since then that you feel like, okay, we need to be a part of this?
[00:13:01] Gina Bartasi: Yeah, I think the biggest thing that's changed is employers now recognize that having a fertility benefit has gone from a nice to have to a must have today there is a robust RFP process.
There wasn't any RFP process. There wasn't anybody to RFP the business too. It was kind of progeny. And then I think you had some legacy players whether that was when or arc, but they really weren't in the employer business like project. You had no competition the first four or five years, and then they've got their hands full.
Now in the last couple of years, there are several kinds of other Progeny me toos, whether you, whether you, you know, again, you see Carey C store club, you see Maven coming in and there they do care navigation. We sit independent from those folks because we're in the provision of care. So we can also do care navigation, which we would argue as table stakes, but really only three things matter in healthcare.
Any kind of healthcare, but specifically fertility patient experience, patient outcome, and cost. It's the only thing that matters to the patient,patient experience, patient outcome and cost. And by the way, it's the only thing that matters to the employer. And what I have found after building and running the largest care navigation firm as a care navigation or middleman or an insurance company, you cannot effectuate change in those three areas, an insurance company, or a care navigation firm cannot affect member experience.
They cannot affect outcomes and they cannot affect costs. Only the doctor's going to set his reimbursement rate. He's only going to decide how many embryos to transfer only. He can decide how to give that patient bad news, whether that's a diminished ovarian reserve diagnosis or a failed IVF cycle, but in order to really effectuate change, And really change kind of how patients go through the process.
You have to be in the doctor business. So today the employers are issuing RFPs. I think in the beginning large tech companies on both coasts are really in the valley, kind of started this fertility benefit. But today you see requests coming in from very, very large employers in retail and manufacturing and automotive.
Like it again, it's moved from kind of a nice to have to a must have benefit.
[00:15:13] Griffin Jones: For that reason though. Wouldn't those other companies say that Kindbody is not independent, that they're independent because they're not in the provision of care and that you're able to manipulate the market. If you end up becoming the Jeff Bezos or the Sam Walton. out there.
[00:15:32] Gina Bartasi: Yeah, well, so we have partner clinics who are very like-minded. We have other clinics that are not like-minded and they don't join our network, but there's a bunch of clinics that prioritize patient care and are very genuine about patient care. And they see a lot of volume from us now, a lot of volume from us.
So I think that concern of okay, if Kindbody sells and directly to the employers, they're going to keep all the business. We have too many other partner clinics willing to attest that that's just not the case. I think in the beginning there was worried, but we've been at this, you know, a year and a half, almost two years now.
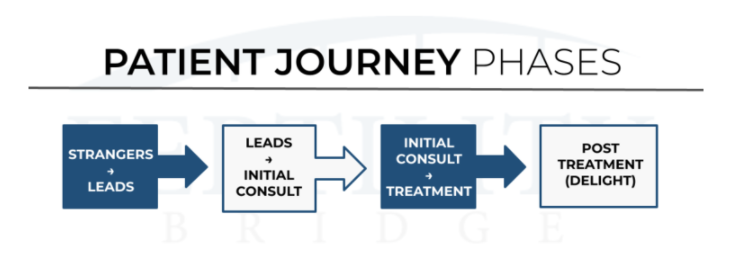
And we have clinics again, that would attest to Kindbody treats is fairly, they pay well, they pay on time. Like there's just too many people out there advocating exactly the opposite. Now our job is to continue to improve member experience every step of the way. And so you know, we prioritize patient experience and we do think we hear from patients the way patients experience and go through that Kindbody journey is very different than many of the other primarily legacy practices.
There are some new clinics, again, that I think are again very like-minded in our peer group that we have a lot of respect for it's mutual, but going through. Kindbody utilizing our proprietary technology is a very different process than a legacy clinic where you fill out a paper chart, the nurse calls, you get your voicemail, you get to call them back.
They get to call you back. They get like all of that waste and inefficiency and telephone tag. That's endemic in the legacy fertility programs, as well as the legacy care navigation from secure navigate. The challenge with the care navigation firms is, you know, once you refer that patient to another clinic, you lose sight of them.
You don't even know if the patient showed for their appointment, much less, whether they had an ultrasound scan and for the employer that they don't even know if they're being double billed, they may have major medical and you could build that for them. You could build the ultrasound scan through major medical.
You could also build the ultrasound scan through your fertility care navigation firm, but there's a lot of waste in healthcare and in the fertility industry that we seek to continue to get rid of and, and operate more efficiently. And I think the employers, and I know the patients see that today, the member experience is significantly different and I use member and patient as the same thing.
Patients are the consumer terminology member is what employers call their consumers or their employees are called members.
[00:18:02] Griffin Jones: So how do you scale this out at a, at a time when REI is, are a bottleneck with 1100 of them in the entire country, we have far more people that need treatment than we have an infrastructure to be able to treat them.
And so how. Are you able to expand how many people are able to be treated? What's the role of OB GYN is, or physician extenders in your model?
[00:18:30] Gina Bartasi: Yeah. You know, I think everybody acknowledges today. You have to have a physician extenders. You just do there's, more than demand than supply.
And the number one thing that hurts a patient is having to wait 3, 6, 9 months for treatment. I would tell you that again, Angie Beltsos says, your question is about scale and how we serve up enough REI is to handle all of the demand that is Angie Beltsos's wheelhouse. You look at the physician productivity of her doctors and it's extraordinary.
One of her lead physicians did more than 1000 cases last year. That's extraordinary. Now you have to have the mindset. You have to have the support around you. You have to have the APP's around you. You know, again, I've spent 12 years in the industry and most doctors, not most, a lot of doctors I've talked to are very comfortable doing 150 cases.
And they say that, listen, I do 12 to 10 to 12 cases a month. I sell an IVF cycle for $25,000. And that's my model. I'm like, okay, well here, our success rates and heres, yours, and I just don't think patients, we have one mission and that is to increase accessibility for all. Fertility treatment has been reserved for rich white people on the upper east side of Manhattan.
And the Bay Area and Beverly Hills, and we think there is something tragically wrong with charging $25,000 for an IVF cycle and insisting on cash pay. We think the model has to change. You have to bring down the cost of care. You can have a premium experience without a premium price tag. Griffin.
The question is, how do you do that? Well, you utilize technology and you use technology to replace everything that's transactional and healthcare scheduling appointment. We are the only fertility clinic that I'm aware of that allows you to schedule an appointment, move an appointment, cancel an appointment.
You can pay your copay. Like everything. That's transactional should not be done by an REI. It should not be done by your front desk manager. It should not be done by your RN. It should not be done by any of those people. It should be done by technology. How do you pay for everything else? You do it online.
Like this industry is incredibly archaic that there's all this telephone tag in doing simple things like paying copays and scheduling an appointment, or even hearing your medication. Like you're walking down the street, you're driving and a nurse calls and says, turn up or down your FSH drug. And you're trying to write and drive and you're, you know, it's incredibly emotional, like all that's bad.
So we own our own patient portal in our EMR. So everything's incredibly transparent. You can pick it up. And by the way, if you forget what the doctor said, you can go right back to your patient portal and remember what the doctor said. So we believe that we can get to scale and extraordinary physician capacity, but we have to have like-minded physicians, the physician that says to us.
I only want to do 10 to 12 cases a month is not the right fit for Kindbody. And if Dr Beltsos says we're on this call, she would say the same thing. And that doesn't mean that we want the physicians working harder. It does simply mean we just want them more efficient instead of taking down the patient's credit card or calling the patient's insurance company to help them understand why same-sex male couple cannot conceive and, and meet the 12 month threshold that your legacy benefits provider has in place.
Like all of that needs to go away so that the REI is doing things only the REI is capable of doing.
[00:22:05] Griffin Jones: So I've got to decide because I'm not Joe Rogan with a three and a half hour format that I've got to decide, which of these four or five sub topics that I want to go down that you talked about. Let's start with the, you know, talk about like, we agree that we're at a point where we have to use advanced providers.
The debate is to what extent. And I just had the CEO of Mate fertility on debating this topic with Dr. John Storment and I don't know if that episode will drop before or after yours, but th but it's very much a debate of to what extent. And so what is the limit of, in your view of where advanced providers can be used or where trained non REI, OB GYN?
[00:22:50] Gina Bartasi: So you should know that I do not make any clinical decisions. I have never made any clinical decisions. I don't make clinical decisions today. Dr. Angie Beltsos our CEO of clinical. We'll make all of those decisions today. We use REI to do all retrievals in all transfers exclusively. Okay. Now we people know Kindbody and the knock is, oh, you guys have OB GYN.
Well, 20% of our revenue is GYN. We do complex GYN, right? I mean, again, what, what, what we don't-we prioritize the patient. Okay. We just do, and we think when you have an ectopic, the worst thing we can do is send you back to a primary care. Or if you have a miscarriage, the worst thing we can do is send you back to some doctor that doesn't have your medical record to go back and do a surgery that can be done by our OB GYN onsite.
You build an affinity with this brand and this REI doctor, you hear patients talk about autonomy. My fertility doctor, now I have to go back to my primary care doctor to get a D&C, like something's wrong with that? That's archaic healthcare that has all these silos and bifurcation. And no one cares about the patient.
Do my medical records follow me from my primary care, from my OB GYN, to my REI, to my mental health specialists, to my nutrition coach. The answer is no, unless you're at con body at Kindbody. We built the entire company around the patient and we said, okay, we're going to blow everything up. We agree that the current model is broken.
It's not anybody's fault. It's just history, right? That's how it was created. The REI set over here and the primary care it's because of how insurance pays for historically didn't cover fertility, but yes, covered major medical and maternity. But today, again, if you prioritizing the patient, the patient doesn't want to be shuffled to all of these different providers.
They just want a baby. They want it as affordably and as nicely and as kindly and as easily and conveniently as possible. And it's not that hard, but it does mean like breaking some traditional rules that says, okay, your OB GYN and your REI cannot be under the same roof together. We think that's silly and not patient friendly.
[00:25:11] Griffin Jones: Well, you talked about as part of that, that you're not going to make these clinical decisions. That's why Dr. Beltsos says she CEO of clinical. And I have to say I'm incredulous when CEOs say this a bit, because to me, it's not like there's not a perfect divide in everything. There's things overlap a bit.
And an example that I was challenging Dr. Andrew Meikle, on this from the Fertility Partners and how he gave an example of client is kind of like one that you talked about that happy doing 150, 200 cycles, the sweetest, sweetest people that really love their patients are definitely not charging them a lot.
Definitely they are below market rates. This individual sees all of their own you know they eat this individual does the ultrasounds for all of the patients. And like to me, that's where, you know, when you're saying like, you know, we'd get rid of these transactional things that the REI does not need to be doing.
That's something that the REI does not need to be doing in my view business guy, Grif that owns no part of his business, but if I own part of someone's business, I think that I would be making that call. And that's an overlap where the standard of care matches with or overlaps with the transactional, isn't it?
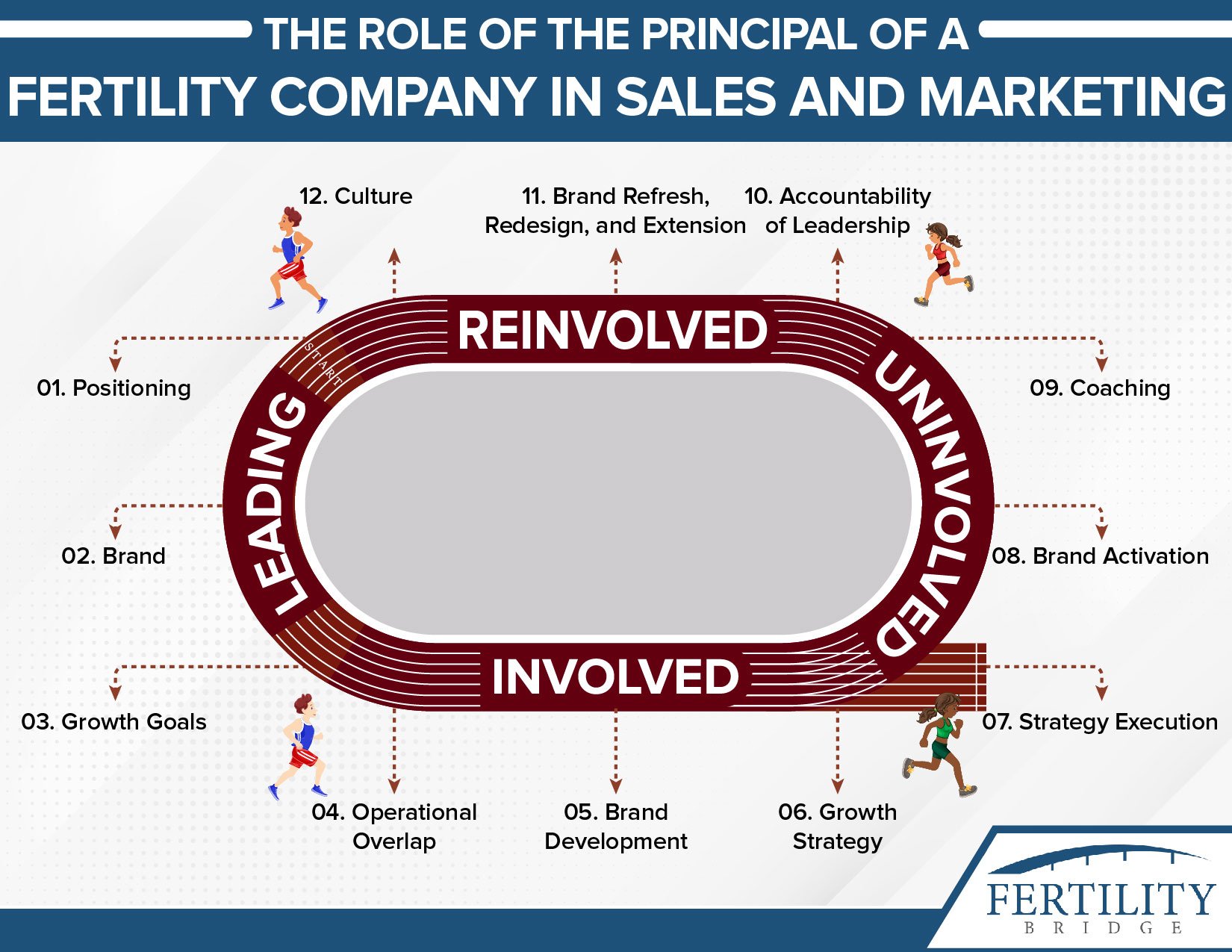
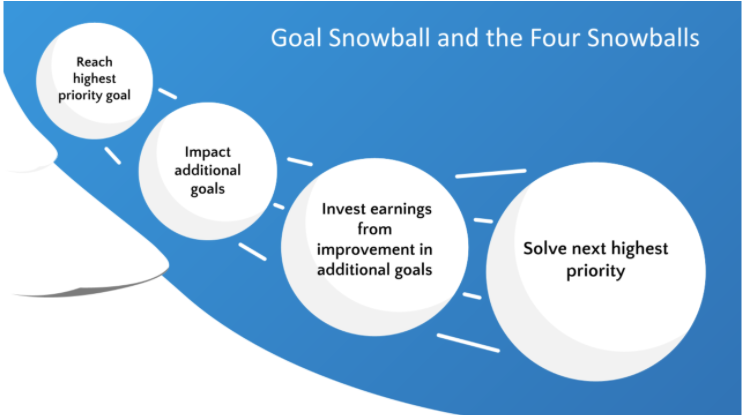
Is a light bulb starting to go off about what branding really is, what its power is that it's not just a marketing tactic done by your marketing director. It's not just done for patient acquisition.
It involves the binding of the culture of what you're able to do, of how patients perceive you and how they want to come along and how your peers and prospective employees and prospective providers. See you, and are you the one that is in line with the current generation? Can you at least communicate to them or are you seeing as something less relevant, something less?
To want to be a part of, if that's the case, did you know that we have a full creative team? We have a creative director, we have an account manager, we have an operational marketing strategy. We have a digital strategy, all full-time people. Plus our production, people that know the fertility, patient marketing journey of not just the creative messages.
But where it goes and have a system, a fertility brand scale that makes it easy for you to not see, okay. It's just us trying to say we should become more current or more hip, more new, but that can actually say, okay, this is where we are at a 1.75. And this is where we want to be at a three point six. We have that all, we have that all Fertility Bridge and to start with us, we're not going to do everything for you at once, but just to look at what you've got and at least tell you what to do.
That's less than $600. It's the goal diagnostic. It's 90 minutes with myself, us giving you this framework and going through what you have and applying that discussion of positioning and branding with you and your partners go to fertilitybridge.com. Sign up for the goal diagnostic and represent your group in a way that is fitting with the practice that you're really trying to build, because I think you might be starting to see that all this brand thing it goes beyond just getting people in the door.
It's who you are. And if you want some help, we're happy to help you with it fertilitybridge.com goal diagnostic. Meanwhile, enjoy this conversation about branding with Gina Bartasi.
[00:28:46] Gina Bartasi: Well, so again, this has to go, this goes back to why Vios and Kindbody were so meant to be like the way that we were practicing medicine. And we thought about ultra sonographers doing ultrasound scans was that's how we were practicing medicine with Vios and Angie, and decided to come together, like how we practice medicine and how we prioritize the patient, how we have phlebotomist draw blood sonographers, do ultrasound scans.
You know, like what nurses do we was just together. Now I will tell you, Angie has upped the game. She's refined the process and we follow her lead. There is no, like, again, an Angie will be the first to say that. And the business people take a back seat and Angie is a business person, but she is our clinical leader.
So she decides patient flow, a number of nurses to REI. She decides all of that. Now, again, the reason that these companies came together so easily, We believe so many things. We were already practicing medicine. It's not like you had to take the client that you just mentioned that was comfortable doing 150 cases a year.
And you had to put that culture with this culture. The cultures went together just like this easily and seamlessly because we already agreed that truthfully, the REI is a subspecialist. This is a well-educated they've been in medical school a very long time. I have a hard time asking any of our REI's ,can you do an ultrasound scan? They'll they will do it. They're happy to do it. They've done it before. It's just, you know sonographers doing 20 ultrasounds a day and REI might, you know, do two a week to help one out. So it goes back to, you know, again, patient how the what's in the best interest of the patient.
Do you want somebody doing this twice a week or 20 times a day?
[00:30:43] Griffin Jones: Well, let's talk about the best interest of the patient with regard to what you were talking about. Like you said, you know, what Dr. Beltsos has been able to do with physician productivity is incredible. I was just talking with just recorded a different episode, different topic.
We're talking about embryologist and it was like, these embryologists are burnt out. Like they can't do any more because, but the demand is that, like, we were trying to get everything we possibly can out of these embryologists. And so there is a tension between what the market needs, the patients need that you're trying to address and what the capacity of the workforce is able to deliver.
You said in the very beginning, something that I don't like when CEOs say Gina and I, cause I try to make myself choose, which is employees come first patients come first, which is declines come first or new employees come first. Do the managers come first? Or the customers come first. And so what, what, like when you're trying to meet a demand and meet the market, and we know that the market demands five times more than what the field's putting out, you're trying to meet that.
How do employees possibly come from first?
[00:31:53] Gina Bartasi: And employees always come first. They have to, because the employees will take care. If you take care of your employees first, they will take care of your customer. They will take care of your patients. And that's when we're talking to doctors, you know, doctors say, well, I used to do that.
You know, we want the doctors to know that we can train and teach nurses and front desk managers and practice managers to be just as kind and just as empathetic to that patient that the doctor can. So again, employees always come first as it relates to the lab. Listen, there's a shortage of labor everywhere.
It's the embryologist, there's a shortage. We know there's a shortage in our eyes. We have to do a better job of training. We've been fortunate, you know, we pay competitively our team members get equity. That's not true for 90% plus of the fertility clinics. And so I do think it was really, really difficult for us to hire the first 12 months, but in the last 12 months there's quite a bit of incoming interest in I've got career opportunities at Kindbody.
[00:33:00] Griffin Jones: So then how, but I used to agree with the employees always come first and I'm trying to like, like actually live that out now. But I used to believe that Mark Spolestra said that we have it wrong, that we put shareholders first, then customer second and employees last, and it should be employees, customers, shareholders, because if you take care of the employees, they'll take care of the customers and now it'll make the shareholders happy.
And I always did believe that until like, but what about when you get to this point that we're at, which is a bit historic, like this labor shortage that we're seeing, not just in the IVF, like every place in the market, but it's like, all right, I can take care of employees till the cows come home.
Anybody's employees can go someplace else. Right now. You're trying to, you're trying to keep them up. And meanwhile, there's so much money in the marketplace that people are coming to you and there's so much demand. And you're trying to like, how do you do that now?
[00:33:54] Gina Bartasi: Yeah. I think again, you have to utilize technology, so you have to go through the lab.
Certainly. That's what we're doing in practice management. So our product people, shadow doctors and nurses to see what they do on a daily basis. That's repeated. Okay. What do you do every single day? That's repetitive. That should be moved to our EMR patient portal or somebody else now what needs to happen that we're probably not doing as good.
A job of Griffin is having our product. People shadow the people in the lab and it has to do with the sterile nature of the lab it has to do with I'm not even sure what it has to do with you know, Dr. Beltsos could tell us, or even Dr. Morbeck Dean Morbeck as our chief scientific officer. But we have to get arduous task and any task that can be moved to technology, to technology, and then you free up human labor.
We've been able to do that on the practice side. We have not spent as much time refining that on the lab and embryology side. I'm optimistic that more economies of scale can come. If you just spend time in the lab and say, what are you doing? That's repetitive. That should be moved to technology.
I do know now we've rolled out some new technology platforms to help kind of ease the burden. And then there's this, like, there's a, there's a training and an input of data and an expert and an export of data that is more time consuming for our embryologist than we would like. But you get through this kind of crunch time of about three months, anytime you roll out new technology or implement a new SAS solution, but we are constantly thinking about.
How we can use technology, whether it's our own or whether it's a third-party vendor to free up humans in this case, embryologist. But right now, embryologists are doing a lot of repetitive things that we think that can be moved to technology. Now, right now they're still biopsying, trifecta, derms, like a lot of their stuff.
They're still you know, cryopreserving oh, sites, they're still doing a lot of things that require extraordinary hand-eye coordination. And those things are, are not close to being automated. But there's still a lot of other things on their plate that can be automated.
[00:36:07] Griffin Jones: Well, let's shift gears a bit and talk about what I really want to talk about, which is this global brand, cause this is the type of stuff that I am interested.
I am interested in brand. I'm interested in creative messaging and I think it is a huge mistake for anybody who thinks is window dressing. That is not looking at it at all correctly. And I want to know if you think that. Maybe exaggerating with this, but I don't think that kind of body could have gone into all of these different angles to the depth that you have without the foundation of the brand that you had built.
Am I overstating it?
[00:36:48] Gina Bartasi: No, but you're a marketer and a brand guy. You sound like me. Like again, we knew it's not fertility, it's not IVF. It was intentional Kindbody wants us as humans to be kind to our body. It also does not uniquely say IVF. It could be egg freezing. It could be same sex. Like there's a lot of things that go into this name and this brand.
And it doesn't say Seattle, it doesn't say Charlotte, it doesn't say any particular city can be a global brand. But we thought about that from the very beginning, because I felt like healthcare was missing a room. Global brand. It's not blue. It's not pink. It's, you know, yellow, we call it optimistic, yellow, yellow is intentionally gender neutral.
A lot of people, if you do all of these customer surveys, which marketing people do a lot of people, don't they just say, here's what I believe. And I'm like, whoa, did you do any research or did you do any customer surveys? But if you do customer surveys on your thoughts about yellow, lots of people associate yellow with happiness, right?
Hope like there's a lot that goes into this yellow and this name and it's intentional. All of our locations is intentional. Do we don't have any hard edges in any of our clinics? There are no 90 degree desk. Everything is round there's again, a lot of thought that goes around this round desk, softening the edges.
There are no medical degrees on the walls. Our REI are highly educated. We don't need degrees from Brown University or Stanford on the wall. You'd probably as an educated patient, know that I went to Stanford or to I didn't. But so we do, we believe there there's huge power in brand and now, you know, We've been fortunate.
There's a lot of affinity for the brand. And so now we try to, we're always working to extend the brand. And so now we are, you know, we spray paint chalk every time we open a location, it's cool to be kind. Right. ‘Cause we have to remember in this busy world, and this is before the war and now there's a war and there's, you know, there's just a lot of challenge.
And so we have to remind people because it's cool to be kind like lead with kindness because kindness is contagious. It's like our yellow happiness, like, you know, just be kind you know.
[00:39:01] Griffin Jones: Brand driven CEOs have such an advantage that you being a brand driven. Like when you look at like, I think Sara Blakely, Spanx, Walt Disney Richard Branson, like these are brand driven CEOs and to you are Kindbody is the furthest end of the spectrum.
I actually have that spectrum, but the other end of the spectrum is people who think nothing about brand whatsoever and say, oh, we have to, oh, that's like a logo, a yeah. Like colors. Yeah. Like have our marketing director just, just do something like that. And it is everything that you do, and it's enabled you to go to, to all of these different places.
And so I want to talk a little bit about like, how that. Moving along with the generations, because, so we made a scale, we made a four point spectrum of the fertility brand and decide on a one. This is your advanced reproductive surgical associates of Smithfield like that, the ones. And then the twos is like Patel, Fertility or, you know I'm trying to make up a Smithfield IVF, very on center.
And then a three is like the nicest of your healthcare brands got a familiar messaging and, and kind of body is the, is one of the only, so we ranked every center in the entire us and Canada kind of body is one of maybe like the only force they one or like one to three fours. And so that, like, you're the first kind of consumer brand in this space.
Talk a little bit about.
[00:40:42] Gina Bartasi: Well, that's intentional. Right? First of all, thank you, Griffin. Second of all, it's intentional. It didn't come after the fact it was we wanted to create a consumer brand, by the way. You know, we also think now, like, and I know Peloton has been beaten up in the public markets, but we think about Peloton instead of soul cycle.
Like, we've talked about how magical Dr. Angie Beltsos says like, how can, how can we get Dr. Angie Beltsos to be Ally Love or Robin Arzon Jess King? Like, how can you, how can you make Dr. Angie Beltsos global, right? And so we are constantly thinking about the brand and about how we protect the brand and how we continue to do right by the brand.
How even in the most difficult, challenging situations, we're kind to each other kind to competitors. We call them peers. Peers is a more friendly term than competitors. So it's in our language, it's in our culture like how we protect each other, how we protect this brand, how we cultivate the brand.
But again, it was very intentional from the beginning when you come to any of our clinics, or even if you go to the patient portal, most patient portals are ugly. Most EMR is, are ugly. Everything when we should, at some point give you a product demo. When you come in to our product through the technology, everything is very elegant.
Everything is yellow. It's on, not everything is yellow because we have neutrals and other colors, but it is aesthetically pleasing, right? And so you can see all these touch points along the way. We predict your likelihood of success. We predict how many eggs we think you're going to get. We predict fertilization rates.
We show your embryos growing. We are completely transparent. And again, when you go into the clinics it's not white, right? There are no white coats. There are no white walls. There's no white paper. 50% of our REI's are BIPOC. I am incredibly proud of that because guess what? Our patients are 43%.
But it goes back between 43 and 50%, but it's intentional. If you really create a mission that says, we want to increase accessibility for all, then you have to have a brand. You have to have visual elements. You have to have clinics that look and speak to accessibility for all. And that's not white walls or white coats or white paper.
[00:43:08] Griffin Jones: It of corresponds with the generations too.
So on our scale, we laid it across the generation. Like, so you picture the generations is like a news ticker, and it's not that a one was, was like one equals baby boomer. It's just that like the overlay of a one is that it was designed or, or lack of design for the baby boom generation. And a two was that baby boomer bit X and three was mostly acts a little bit millennial. And so the fours, which you're one of very few as is the the first brand that's for millennials and gen Z
[00:43:49] Gina Bartasi: Yeah. Yeah. Again, a large portion of our new patients come from Instagram, look at Dr. Beltsos or Ruby Jelani or any of our doctors. And, and we encourage them to do that.
Like we are kind, but we're also fun and competitive and we're like, okay, who can, you know, create our competitions? Like could be great. The funniest Tiktok video, like, I don't know, we're having fun, practicing medicine, helping our patients build the families of their dreams and that doesn't have to be white and sterile and old, right.
It can be fresh and it can be fun. And so, you know, when we think about brand, we have competitions of who can create the most fun tick-tock video. The majority of REI is that got your one, two, and maybe even some of your threes are like Tiktok, like, is that tic-tac-toe what is Tiktok? You know? And so, but we are constantly thinking we want to be better than we are today.
All of us do. That's the competition in us. Okay. We have an extraordinary brand today. Like how do we take it up a notch? And we're trying to think about what's happening new on, on Instagram. And do we call our locations like as a con body ATL, is, is it Kindbody Bay Area? Do you start then to segment these markets or is it just one brand?
But we think about brand every single day. We think about culture every single day.
[00:45:14] Griffin Jones: Talk about how those two are, are together, because I'm trying, I'm just finishing an article called the difference between Brandon and called where they, where they converge and where they diverged. And so I think like so many, I'm finally starting to get people interested in branding and creative messaging for like how they set expectations with their patients and how they get their team to be cohesive around something, as opposed to, they don't care about patient acquisition right now, because everybody's slammed.
That's how I started in this marketing field was marketing patient acquisition, but it's like, no, this is how you get people and like it as a part of something. So I want you to talk about the culture, cause I'm thinking like Gina, before I look at somebody's LinkedIn profile to like, see what they're, I know that they went to work for cause it seemed in the yellow, in the background.
And so talk a bit about how you use the brand for culture.
[00:46:12] Gina Bartasi: Yeah, I think a lot of it starts with humility, right? The brand is humble. It's not, anybody's last name. It's not, you know and our culture really starts with this humility. Right? So those two things are ingrained. I think that's not just humility too.
It's a vulnerability to it. You know, it's also our brand and our culture. We do embrace risk. You know, we tell our doctors so I can brace risks, do something crazy on TikTok. And you tell a doctor or a scientist embrace risks. They're like, whoa, whoa, whoa, whoa, whoa. I'm a doctor. I don't embrace risk, except that if you teach them, we're not talking about embracing risks.
When it comes to a prognosis of an onco patient, we're talking about taking risks as it relates to the brand, as it relates to culture, allow yourself to have fun. Allow yourself to smile, giving devastating news, another failed pregnancy test is hard. It's hard. And we're so glad you're empathetic to your patient.
But outside of that, how can we make you smile? How can you be cheery and yellow and optimistic? And so we believe that there's a lot of similarities that brand and culture do go together. And I don't think our brand would be as successful if our culture wasn't so strong. And I don't think our culture would be so strong if our brand wasn't so strong.
And I think the other thing that I would say about culture and brand is team, right? I think too often, you know, healthcare, people and doctors in particular may think solo first, like I'm a doctor and at hierarchical and solo, and those are not things that belong in our brand or our culture.
We don't do anything singularly. Not any of us. And Dr. Beltsos would say the same thing and Beth Eschbach Greg Poulos, none of us do anything by ourselves. And that's intentional. We make group collaborative decisions and same thing with our brand. It's we invite feedback. We invite constructive feedback, constructive criticism, because we want to get better every day.
And again, that goes back to our brand and our culture.
[00:48:15] Griffin Jones: And with recruitment too, I have to believe that that's giving you an edge because just look at, you, look at a one baby boomers. Who's answering your phones. Who's not even the answer who are the docs now who's buying in. And so I have to believe that, you know, it's like in these places that are like, oh, you know, we're busy as can be with.
New patients, but what is it like with people that like, do they want to come work for you? Like are they excited about, are they behind a mission together that they will go and express to their friends of like, this is who IVF and worked for and you better know about them.
[00:48:53] Gina Bartasi: They are. And they do.
That's recent though. It's just in the last 12 to 18 months. You know, Dr. Lynn Westphal was our first REI and our chief medical officer. And it was hard even with Lynn's reputation and, and she has an extraordinary reputation and is a member of SARC, a legacy member of A\SRM and starting a phenomenal reputation.
But remember doctors I said are notoriously risk-averse. You encourage them to take risks and not like, whoa. And so in the beginning they Kindbody was, you know, another startup and, you know we started in a mobile clinic that was oriented towards the brand and service. We're going to bring care, whoa, Griffin, we're going to bring care to the.
You don't have to come to me. I'm going to come to you and the doctors like, whoa, whoa, whoa, whoa. You have a mobile clinic. You're going to the patient. We don't do that. Patients come see me. They wait months to see me. And I'm like, why are you bragging about patients waiting to see you? Like something's unconscionable, but a doctor would brag that you're you have these long wait lists.
Don't stop bragging, stop bragging. It's not good for the patients so.
[00:50:01] Griffin Jones: That's thinking like an individual contributor as opposed to an entrepreneur though, because the entrepreneur wants to scale the individual contributor wants. Yeah. It's like, oh, sweet. I'm the best.
[00:50:12] Gina Bartasi: Yeah, well, and again, I think now we have, if you count all of our providers, the APPS, the REI's the OB GYN, there's 65 or 70 of them.
Now, maybe it's 75 or 80, I'm losing, but there's enough now in the industry that they do call, you know, they do call and say, Hey, it'sKindbody hiring. We have in our slack channel, we have a new hire and there's a big referral network through the doctors in the embryologist. So it's gotten significantly easier in the last 12 to 18 months.
And then again, you look at these extraordinary leaders on the clinical side and again, both our scientific lab site, as well as our practicing.
[00:50:53] Griffin Jones: I know the criticism that I'm going to get after this episode, which is I've been blowing sunshine for Kindbody for the last 15 minutes. And so no, I'm not because one, I can't evaluate you on a clinical level.
I'm not qualified to do that ever. And and even I'm not qualified to evaluate you all on many of the areas of, of your business model. I don't know. I don't know if they're a good or bad what my wheelhouse is brand and creative messaging. And for those of everybody listening knows that that's what I care about most.
And I'm not making this up, you could look at our scale. If you want, you can look at our spectrum. It's empirical kind of body is a four on that. And I think it is a huge advantage that the other networks don't have. Again, oh, you're blowing sunshine. No, I'm not. This is an advantage.
The other networks have a disadvantage of your there IGA. If anybody remembers the IGA soup or like a True Value, they bought hardware stores. Where kind buddy has the Starbucks advantage. I think it's such a disadvantage for these networks that are, that are going for scale to not have any of the advantages of scale that come from brand, which is not window dressing for all of the reasons that we just talked about the instead of it's we're Joe's coffee in Seattle brought to you by we're we're coffee roasters of Denver brought to you by so-and-so over here versus Starbucks where Starbucks, where Starbucks and that there's something about that, that, that pretty lady in green that you invites the customer to be able to recognize something that unites them, to be able to express it themselves, as opposed to just someplace else and the employees that want to and do work for there.
It's like, this is what we're about. And so when did that, when did you know that that was going to be a thing? Like when did you think about doing it the other way at first? Like, oh, well maybe we'll be a network.
[00:52:50] Gina Bartasi: No, we were always going to establish a brand. We were always going to have these warm colors.
We had three focus groups, three dinners and three focus groups. So six meetings and we would pull the audience. Do you like yellow? Do you like purple? Do you like warm? Do you like hard edges? Do you like blue? Like. And this brand is where it is because we gave the brand to consumers, to future patients, to existing patients and future patients.
And this was before COVID, you know, we had in-person meetings, we sent out surveys. We still survey patients. We want to know, because I think if you, you establish a brand three and a half years ago, you ought to check in on it every four to six months to say, Hey, am I on the right track?
We do. We measure NPS. We are maniacal. We have a 90 NPS, which is unheard of in the healthcare field. It's definitely unheard of in the fertility field, but we measure every single we want to know from patients how we're doing. We want to know that patients have this affinity for the brand. Doctors and nurses and our front desk team to fill an affinity and a protector of this brand.
So, you know, thank you for the accolades and the kudos. If you were able to measure our clinical success rates, like we have a responsibility to report to the CDC and SART you will see that they are above the national average. Now they're above the national average because we're big proponents of GPTA, but they are in line with our peer group.
And I think that was, you know, everybody said, okay, you can build a brand, but maybe your clinical quality would have to sacrifice, oh, well, you know, how are you able to offer an IVF cycle at 25 to 30% less than everybody else? Like you use technology, you know, Dr. Nicole Noyes just joined Kindbody and New York and you and patients are now going to be able to see Dr. Noyes at 30% less than they were paying at Northwell at NYU. Okay. I am ecstatic about that. I am so happy for a patient because many patients that 30% additional charge would have been out of reach, much less patients that have to go through two or three or four cycles. So we continue to be on a mission to provide more accessibility for all a premium experience, without a premium price tag.
[00:55:15] Griffin Jones: I want to say something about somebody that I've been reluctant to say that about two other companies too. And the reason I haven't said this is either in an article or on the show is because I think that people will either think that I'm insulting them or that I'm propagating them. And I'm really not doing either.
I'm really just saying mucho ojo pay attention, like really pay attention to what they're doing. That I don't feel get enough respect and what, so I've made, like I'm saying, I don't feel like they get enough respect. What I mean is pay attention. And that's you all it's Fertility IQ at CNY Fertility. And and so like where you are in this journey.
I don't remember if it was Nelson Mandela or Desmond Tutu, who that says, you know, first they ignore you, then they laugh at you, who then they fight you, then they join it. Where do you feel you are on that trajectory?
[00:56:05] Gina Bartasi: It's hard to group everybody in the same bucket, because I think, you know, the end, I think some are still fighting.
Some have already joined and then some are still making fun of us. Despite our clinical success rates. Despite we have 84 clients, they're fortune 50 customers. They're big blue chip customers. You know, we have a sign in every single Kindbody location. And as we have lots of art, because we think art goes back to the quality of the brand, but there's a sign that says underestimate me.
That will be fun. And so, listen, we don't mind, like I I've had a lot of criticism throughout my career. You get tougher at it. You get accustomed to the criticism because you're doing something new. So underestimate me. That'll be fun.
[00:56:59] Griffin Jones: What is on the horizon for you all? What is Kindbody need to accomplish in the next year or, and more interesting like what's going to happen next with the brand?
[00:57:13] Gina Bartasi: You know, again, we've talked a little bit about it, but I think you'll see the brand globally. And I think you're going to see the brand more and anything Griffin, where we let go of the patient, if you prioritize the patient, but then you send the patient out for genetic testing, or you send the patient out for carrier screening, or you send the patient out for donor egg or donor sperm or surrogacy.
When we let go of our patient, that makes us nervous because we are maniacal about patient care. And we're not sure that all of the other people that we're referring the business to are as patient-centered as we are. Yes. We trust them, are they're our partner today, but I do think you'll see us extend the brand to other ancillary businesses where we may be outsourcing.
Now we're going to pull those services in house. You know, I want us to be a leading brand amongst same-sex men, amongst single moms by choice. We've done a really great job. I was going to say same-sex women, but we have a lot of same-sex women, men that trust this brand, but I just want it. I, again, we're, we're so oriented towards this mission to increase accessibility for all.
[00:58:21] Griffin Jones: Why didn't venture come into this before? So when I have David Sable on this show, we talk about private equity. They're buying clinics, it's their model to buy a clinic. Venture capital is looking for something that will scale. So they're normally looking at like AI or software, you know, other, other kinds of tech because they want that scale.
And many of them don't feel like, oh yeah, clinic model is something that we can scale. What how were you able to pitch this to venture to say, oh yeah, this isn't a private equity play. This is actually something that we can scale.
[00:58:54] Gina Bartasi: You know, it probably goes back to track record.
I think venture capital people are fearful of CapEx, heavy businesses, like standing up for wall clinics, you know, before we hired a single doctor or stood up a clinic, we own our own technology. We invest in it. We have 55 engineers and engineering and it and dev ops. So there is definitely a tech play.
It's one of the reasons our doctors can be more efficient. They can see more cases because we're not doing all the menial work. I know the VC community, you know, and, and so it was significantly easier this time to raise money than it was five years ago or 10 years ago. So, you know, venture investors, all institutional investors, like pattern recognition and they say, oh, you know, gene has been able to do this before genus, you know, this is Kindbody is my third company and women's health.
It's my fifth startup, which just means I'm crazy. But you know, crazy fun. Like , it does get easier. You're able to build teams easier. You're able to raise money easier. You know, Kindbody has challenges like every other business that's growing has challenges. But today, when we see a challenge versus 10 years ago, in many cases, I know the answer, or I know the person who knows the answer versus when you're just younger or you're a newer entrepreneur.
You spend a lot of time evaluating the answer to that question that was just posed today. Questions and problems come up, but I'm like, oh, I've seen this one before. Here's what we should do. You know, and same thing with Dr. Beltsos and Beth Eschbach or Greg or Lynn or any of our team, like you have an incredibly experienced team with a long depth of knowledge and scaling other organizations.
And that's one of the things that's allowed us to execute this quickly in the short amount of time. This well is a Testament to the experience to this team. If Dr. Beltsos and I tried to do this 12 years ago, when we first met at PCRs and she had all these Christian Louboutin on, like, I am in love with this woman, I don't think we would have been as successful 12 years.
It'd be interesting to ask her that, but 12 years ago, we just didn't have that same level of knowledge of experience.
[01:00:59] Griffin Jones: That's why my client services firm is completely cash growth because this is my learning speed. Yeah, no like it's my learning speed. I will probably do faster things in the future, but I'm really trying to nail the fundamentals right now.
And cash growth has allowed me to do that. So for those that raise so much money and do it so quickly, it's a.
[01:01:25] Gina Bartasi: Well, I don't know how old you are Griffin, but let's assume that Dr. Beltsos, so are at least a decade older than you. And that's the experience I'm talking about. So does that help.
[01:01:36] Griffin Jones: Help there's hope for the rest of us?
I will let you conclude, you know, our audience is REI, is its fellows. It's practice owners. There are a lot of PE and venture people that pop into this podcast when they're doing their, all of their due diligence and studying of the field. So how do you want to conclude to that audit?
[01:01:58] Gina Bartasi: Yeah. We've been incredibly blessed and I just want to thank I think the criticism makes us stronger and makes us better. And then those that have been huge, enormous cheerleaders. Thank you. Thank you, Griffin. It's been great for you to come to the industry as well and really elevate marketing.
I was a marketing CEO, a brand CEO, and so it's good to have other cheerleaders that talk about marketing and brand in the field. So thank you. Thank you. We've been blessed and.
[01:02:25] Griffin Jones: With the field was crying out for a D student to come in and build a client services firm slowly.
[01:02:32] Gina Bartasi: Love it. Thank you, Griffin.
[01:02:34]Griffin Jones: Thanks for coming on. I appreciate it. Take care. Bye.